Radiologist University: Understanding Radiologist Qualifications and Training Pathways in the UK
Introduction
In this article, “Radiologist University” describes the formal sequence of qualifications, exams and supervised clinical training that prepare doctors to practise as consultant radiologists in the UK. Knowing this pathway helps patients, referrers and junior doctors judge clinical competence, subspecialty fit and the likely standard of imaging interpretation for specific problems. Readers commonly ask how a medical degree leads to postgraduate training, what the FRCR exams involve, and why the Certificate of Completion of Training (CCT) matters for specialist recognition. This guide walks through each credential, the typical timeline (Foundation → ST1–ST3 → FRCR → CCT), and how subspecialisation — for example cardiac or women’s imaging — changes later training and local service provision. We also cover ongoing professional development (CPD), the practical role radiologists play in diagnostic services, and how specialist training maps to what a local clinic can deliver. Terms such as FRCR, RCR, GMC, CT, MRI and NATA accreditation are used to link training milestones to everyday imaging outcomes.
What Are the Essential Qualifications to Become a Radiologist in the UK?
Becoming a radiologist in the UK combines a primary medical degree, structured postgraduate specialty training, success in the Fellowship of The Royal College of Radiologists (FRCR) examinations, and award of a Certificate of Completion of Training (CCT), followed by specialist registration with the GMC. Together these elements show clinical knowledge, practical imaging competence and regulatory approval needed to report diagnostic studies and perform image-guided procedures. The pathway balances written exams with workplace-based assessments so new consultants meet patient-safety and diagnostic-quality expectations. Below is a clear comparison of the main credentials and their roles.
Which Medical Degrees and Certifications Are Required?
A primary medical degree (for example MBBS or MBChB, or an accepted international equivalent) is the starting point for postgraduate training. After foundation years, doctors enter specialty radiology training where workplace-based assessments, case discussions and logbook evidence build modality-specific competence. Registration with the General Medical Council (GMC) is mandatory to practise in the UK and underpins later specialist recognition. These steps ensure a regulated progression from general medical practice to qualified radiology provision.
Intro to credentials table and purpose
This table shows how academic qualifications, formal exams and regulatory registration combine to certify a radiologist’s readiness for clinical practice.
What Is the Fellowship of The Royal College of Radiologists and Its Requirements?
The FRCR is a staged exam suite run by the Royal College of Radiologists that assesses radiology knowledge and clinical application at key career points. It usually starts with physics and anatomy/clinical knowledge papers and progresses to clinical reporting and viva components that test image interpretation, decision-making and practical judgement. Candidates typically complete parts of the FRCR while progressing through specialty training; passing the FRCR is a recognised marker of radiological competence and reassures employers, MDTs and referrers that the candidate meets national standards.
Summary of why FRCR matters
Put simply, the FRCR is both an academic and professional milestone: it confirms core expertise and helps trainees move from supervised practice toward independent specialist roles. For patients and referrers, FRCR success reduces uncertainty about a clinician’s ability to interpret complex imaging; for trainees, it provides clear checkpoints that guide subspecialty decisions.
FRCR Examination: A Review of Evidence for Radiologist Training in the UK
The Fellowship of the Royal College of Radiologists (FRCR) examination is a key part of UK radiology training. It evaluates the knowledge and skills needed for safe, effective practice and has been reviewed to ensure its validity and reliability in assessing trainees.
The Fellowship of the Royal College of Radiologists (FRCR) examination: a review of the evidence, TC Booth, 2018
How Does the Radiology Specialist Training Pathway Work in the UK?
Specialty training moves doctors from foundation years into higher specialty training where staged responsibilities, workplace assessments and the FRCR exams structure progression toward the CCT. Training is arranged in clear stages (ST1–ST3) with growing autonomy, defined competencies and increasing exposure to modalities such as CT, MRI and ultrasound. Each stage has typical timeframes and assessment expectations that together form a realistic route to consultant-level practice. The timeline below summarises the usual milestones trainees achieve on the way to specialist registration.
What Are the Stages of Specialty Training from ST1 to ST3?
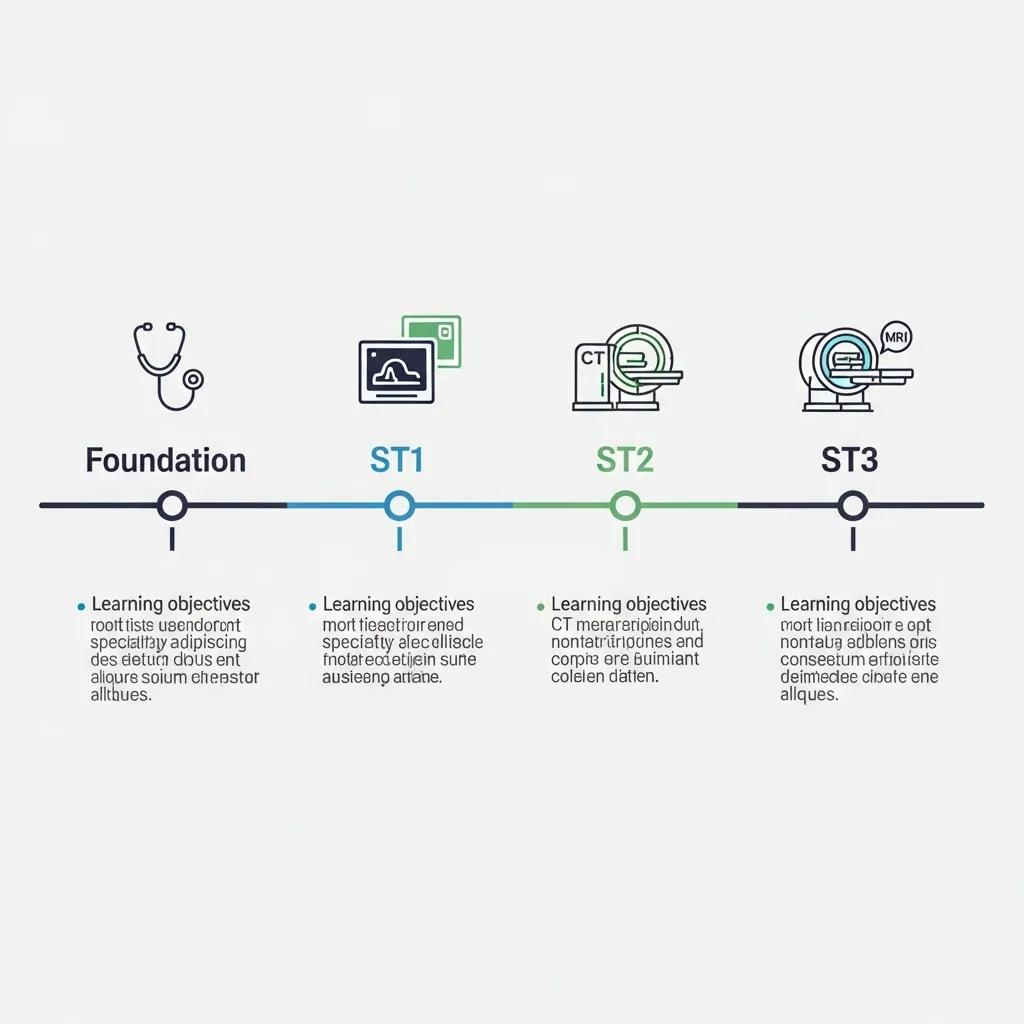
Specialty training normally starts at ST1 with supervised rotations and basic radiology exposure, then proceeds through ST2–ST3 where trainees build reporting volume and procedural competence. The mid-stages are where most FRCR parts are completed and assessed reporting lists are accumulated; trainees begin on-call duties and refine modality-specific skills. ST3 is a consolidation year: trainees demonstrate readiness for independent consultant practice, finish workplace-based assessments and complete the portfolio evidence required for a CCT. Individual timelines can vary with out‑of‑programme time or extra fellowships, but the staged approach sets clear competency targets.
Timeline list for featured-snippet intent
- Foundation Training: Broad medical rotations and core clinical skills.
- Entry to ST1: Start of specialty radiology training with supervised imaging work.
- Mid Training (ST2–ST3): Complete FRCR exams; increase reporting and procedural experience.
- Final Training (ST3): Consolidate subspecialty skills and finish assessments for CCT.
How Do Subspecialties Influence Radiologist Career Development?
Subspecialisation — for example cardiac radiology, women’s imaging, interventional or paediatric radiology — usually follows core training and often involves fellowships or focused attachments. A chosen subspecialty shapes the mix of modalities a radiologist masters: cardiac imaging emphasises cardiac CT and MRI, while women’s imaging focuses on mammography and breast ultrasound. It also influences where consultants work and which MDTs they join. Subspecialty expertise improves diagnostic precision for complex cases and adds value within multidisciplinary pathways, helping clinicians make better, faster treatment decisions.
Summary of pathway and subspecialty impact
Knowing the ST1–ST3 timeline and how subspecialisation affects training helps referrers and patients anticipate the level of expertise available for particular imaging requests and procedures.
UK Radiology Training Pathways for International Medical Graduates: Training and Subspecialties
This review outlines routes for International Medical Graduates (IMGs) who wish to train as radiologists in the UK. It covers the structure of radiology training and the common subspecialty options available to overseas clinicians.
Radiology Pathways in the United Kingdom for International Medical Graduates, 2025
Why Is Continuous Professional Development Important for Radiologists?

Continuous Professional Development (CPD) is essential to keep diagnostic skills sharp, adopt new imaging technology and meet revalidation standards. CPD covers courses, audit, peer review, conference attendance and hands‑on updates — all of which maintain and extend clinical competence. With rapid advances in imaging (for example advanced MRI sequences, AI triage tools and hybrid imaging), regular learning directly improves a radiologist’s ability to deliver accurate, timely and clinically useful reports. The sections below outline CPD activities and how continued training benefits patient care.
What Are the Key Components of Radiology Professional Development?
CPD typically blends structured learning (courses and conferences), workplace activities (audit, peer review, teaching) and formal appraisal or reflective practice for revalidation. Activities are logged as CPD credits and mapped to professional standards so clinicians can demonstrate maintenance of competence. Audit and peer review close the quality loop by identifying reporting variation and driving improvement. Together, these elements keep radiologists up to date with guidelines, protocols and safety processes that support high-quality imaging services.
Benefits list and summary
CPD delivers clear, measurable benefits in radiology:
- Improved diagnostic accuracy: Regular training sharpens pattern recognition and reporting skills.
- Faster technology adoption: CPD supports safe use of new modalities and AI tools.
- Better patient safety and quality: Audit and peer review reduce errors and standardise reporting.
How Does Ongoing Training Impact Diagnostic Accuracy and Patient Care?
Ongoing training helps close gaps identified by audit, introduces evidence-based protocol updates and teaches techniques that increase sensitivity and specificity for particular conditions. For example, focused CPD in breast imaging or cardiac MRI can improve detection rates and reduce false positives through refined criteria and post-processing skills. Regular participation in MDT meetings and case-based learning also aligns imaging reports with clinical management, ensuring radiology supports timely, effective patient pathways and reduces uncertainty for referrers.
Summary of CPD’s effect
In short, continuous learning is both a regulatory safeguard and a direct way to improve outcomes — higher accuracy, quicker adoption of useful tools and clearer communication with treating teams.
European Guidelines for Radiologist Staffing, Education, and Training Standards
This guidance summarises staffing and training recommendations developed by the EU‑REST project, including suggested training durations and the ESR European Training Curriculum for Radiology as a continental standard.
Guidelines and recommendations for radiologist staffing, education and training, M Hierath, 1999
What Role Do Qualified Radiologists Play in Diagnostic Imaging Services?
Qualified radiologists interpret imaging, perform image-guided procedures, advise clinical teams and take part in multidisciplinary decision-making. Their expertise directly affects diagnostic accuracy, treatment planning and patient safety. Radiologists integrate clinical history, current imaging and prior studies to produce reports that guide care and escalate urgent findings when needed. Their procedural skills support minimally invasive treatments, and subspecialist insight helps choose the best modality and protocol for each clinical question. The section below explains why this expertise matters and how radiologists work with referrers to improve outcomes.
Why Does Radiologist Expertise Matter for Accurate Medical Imaging?
Expertise improves interpretation through pattern recognition, clinical correlation and awareness of modality‑specific pitfalls — all of which reduce false positives and negatives that could change management. Subspecialist review in areas like cardiac or women’s imaging can refine diagnoses, suggest targeted follow-up and, in complex cases, change treatment plans (for example by identifying subtle MR findings that affect surgical decisions). This shows how depth of training translates into real patient impact.
Transition to collaboration paragraph
Expert reporting is most effective when paired with strong communication from referring clinicians; clear clinical questions and timely dialogue ensure imaging answers the right problem and that urgent issues are actioned quickly.
How Do Radiologists Collaborate with Referring Doctors?
Radiologists collaborate through structured reports, direct consultations, MDT meetings and image‑sharing systems to align findings with treatment decisions. Standardised report templates and urgent notification protocols help referrers act on critical results without delay, while MDT discussions integrate imaging into care plans for cancer, cardiac disease and other complex conditions. Referrer tools such as eReferral systems and secure image access streamline requests and support efficient clinical workflows, reducing delays that could affect patient care.
Business bridge and short CTA
High-quality radiology relies on specialist training plus efficient referrer workflows. Clinics that combine subspecialist expertise with easy referrer access provide clearer, faster diagnostic pathways. Life Medical Imaging Central Coast focuses on patient care, subspecialist women’s and cardiac imaging, and practical referrer resources to integrate imaging into clinical workflows. To book or enquire about services, clinicians and patients can contact Life Medical Imaging Central Coast via our website or check our local business profile for clinic details.
Who Are the Expert Radiologists at Life Medical Imaging Central Coast?
Life Medical Imaging Central Coast’s team brings together qualified radiologists and skilled support staff who deliver a broad range of advanced diagnostic and interventional services. We emphasise NATA accreditation, a full suite of modalities (CT, X‑ray, ultrasound, cardiac imaging, body composition, bone densitometry and interventional procedures) and subspecialist services in women’s and cardiac imaging as key trust signals. This organisational profile helps referrers and patients link the training and credential concepts above to the clinic’s local capabilities and quality controls. Below is a practical mapping of services to clinic capabilities and accreditations.
Intro to clinic services table
Summary mapping
This table connects the clinic’s services to practitioner skills and accreditation, showing how formal training and subspecialty focus translate into practical diagnostic capability for local patients and referrers.
What Are the Qualifications and Specialisations of Our Radiologists?
As an organisation, Life Medical Imaging Central Coast highlights a team-based mix of qualified radiologists and support staff offering subspecialist women’s and cardiac imaging alongside general diagnostic services. We use NATA accreditation as a visible quality marker and provide referrer resources such as eReferral and secure image access to smooth workflows. While individual credentials (for example FRCR or CCT) sit within the wider training framework described above, our clinic-level summary demonstrates how collective expertise supports modality-specific services without listing personal details.
Schema and profile recommendation
To improve referrer visibility, the clinic can use structured schema for organisation and service profiles to communicate subspecialties and accreditations; this structured data helps map relationships (clinic → service → subspecialty) for better discovery in clinical directories and search results.
How Does Our Team Ensure Excellence in Diagnostic Imaging?
Excellence comes from combining modern imaging equipment, subspecialist clinical oversight and quality-assurance processes such as audit and peer review. These mechanisms mirror CPD principles and regulatory expectations that maintain high standards. Our use of NATA accreditation and referrer tools like eReferral and image access supports reliable workflows, while patient-centred practices — attention to comfort and clear communication — reinforce diagnostic confidence. Ongoing internal review and active engagement with referrers keep our imaging protocols and reports clinically relevant and up to date.
Summary of clinic QA link to patient outcomes
By mapping training, accreditation and technology to concrete processes, we convert specialist radiology competence into dependable diagnostic results that referrers and patients can trust.
How Can Patients and Referrers Choose the Right Radiologist or Imaging Centre?
Selecting the right radiologist or imaging centre means checking qualifications, subspecialty fit, accreditation, available technology and referrer support. A simple checklist helps patients and clinicians make informed choices that reduce diagnostic uncertainty and match imaging to clinical needs. The checklist below lists practical criteria to evaluate providers; after that, we explain how Life Medical Imaging Central Coast meets those standards.
Intro to checklist
- Qualifications and certification: Look for evidence of specialist training, recognised exams and appropriate registration.
- Subspecialty experience: Choose centres offering focused expertise for condition‑specific imaging (for example cardiac or women’s imaging).
- Accreditation and quality assurance: Prefer clinics with recognised accreditation and routine audit processes.
- Technology and modalities: Confirm access to relevant imaging (CT, MRI, ultrasound) and modern protocols.
- Referrer support and access: Check for eReferral options, secure image access and clear communication channels.
Checklist summary and next steps
Using this checklist helps match the clinical question to a provider’s strengths. When a subspecialist opinion is needed, prioritise centres that list dedicated services and referrer workflows to ensure timely, actionable reports.
How Does Life Medical Imaging Central Coast Support Patient Comfort and Diagnostic Confidence?
Life Medical Imaging Central Coast meets the checklist standards: NATA accreditation for quality assurance, modern imaging across CT, X‑ray and ultrasound, dedicated women’s and cardiac imaging pathways, and practical referrer tools such as eReferral and image access. We also focus on patient comfort and a skilled clinical and support team to enhance the imaging experience and diagnostic reliability. For appointments or enquiries, please use the clinic website or our published business profile to contact us directly.
Final note and invitation to enquire
Choosing an imaging provider based on qualifications, subspecialty fit and accreditation reduces diagnostic risk and supports better outcomes. Life Medical Imaging Central Coast positions its services and systems to meet these selection criteria and welcomes enquiries through our official channels.
Frequently Asked Questions
What is the typical duration of radiology training in the UK?
Radiology training in the UK typically takes about 5 to 6 years after medical school. This usually includes 2 years of foundation training followed by approximately 3 years of specialty training (ST1 to ST3), during which trainees sit FRCR exams and complete workplace assessments. Individual timelines can change with out‑of‑programme time or extra fellowships.
Are there opportunities for international medical graduates to train as radiologists in the UK?
Yes. International medical graduates (IMGs) can train in the UK but must ensure their qualifications are recognised by the GMC and may need to complete the PLAB assessment. Once registered, IMGs can enter foundation training and apply for specialty training provided they meet the entry requirements and standards.
What role does technology play in modern radiology training?
Technology is central to modern radiology training. Trainees learn on advanced modalities such as MRI, CT and ultrasound and increasingly use simulation and AI‑assisted tools to refine interpretation and procedural skills. Ongoing updates in technology make CPD essential so radiologists remain confident with the latest techniques and equipment.
How do radiologists ensure patient safety during imaging procedures?
Patient safety is maintained by following established protocols, minimising radiation exposure, and completing appropriate patient assessments before procedures. Continuous training in current safety standards, audit and peer review all support safe practice. Radiologists also work closely with multidisciplinary teams to manage risks and ensure timely, accurate diagnoses.
What are the benefits of subspecialisation in radiology?
Subspecialisation improves diagnostic accuracy and patient care. Radiologists who focus on areas such as cardiac or women’s imaging develop deeper familiarity with specific disease patterns and imaging nuances, which leads to more precise reporting and targeted management recommendations. Subspecialists also add value in MDTs and complex care pathways.
How does the FRCR examination impact a radiologist’s career?
The FRCR is a major career milestone. Passing the FRCR demonstrates core radiology competence and is a key requirement during specialty training. It supports entry onto the specialist register and reassures patients and referrers that the radiologist meets recognised national standards.
Conclusion
Understanding the qualifications and training pathway for UK radiologists helps patients and referrers choose services with confidence. Recognising the roles of credentials like the FRCR and the CCT, and the importance of ongoing CPD, highlights the profession’s commitment to safe, accurate imaging. For more information about our services or to connect with our team, please visit our website.

