Comprehensive guide to X‑ray equipment: types, benefits and clinical uses
X‑ray equipment covers a family of diagnostic tools that use controlled ionising radiation to reveal the body’s internal structures. These images help clinicians diagnose fractures, chest disease, dental problems and more complex anatomical conditions. This guide explains how common X‑ray technologies work, why modern digital and low‑dose systems improve patient care, and which clinical questions each modality best answers. You’ll find practical overviews of digital radiography (DR), portable X‑ray units, computed tomography (CT) including low‑dose CT, panoramic dental imaging (OPG) and bone densitometry, plus clear preparation steps for patients. We link device mechanics to clinical benefit, compare digital radiography with traditional film methods, and set out what patients and referrers can expect before, during and after an appointment. The guide also summarises how advances such as improved detector sensitivity, smarter image processing and iterative reconstruction lower radiation while keeping diagnostic quality high. Finally, there’s a clinic‑focused section detailing the X‑ray services available locally through Life Medical Imaging Central Coast and how to book or refer.
Comprehensive X-Ray Equipment Guide: Types, Benefits & Clinical Uses
Contemporary medical imaging uses several X‑ray‑based device categories that serve complementary diagnostic roles — from simple 2D radiographs to volumetric CT and specialised dental captures. Each type differs in detector design, geometry and clinical scope, which affects image resolution, radiation dose and typical indications. Understanding these categories helps clinicians choose the right test and helps patients know what to expect. The main types you’ll encounter are digital radiography (DR), computed tomography (CT), portable X‑ray systems, dental panoramic imaging (OPG) and bone densitometry (DEXA), with fluoroscopy used when real‑time imaging is required.
Digital radiography, CT and dental OPG use different detector technologies and workflows that influence speed and diagnostic yield. The sections below explain how DR works and where portable systems are most useful to improve access to imaging.
How does digital X‑ray technology work?
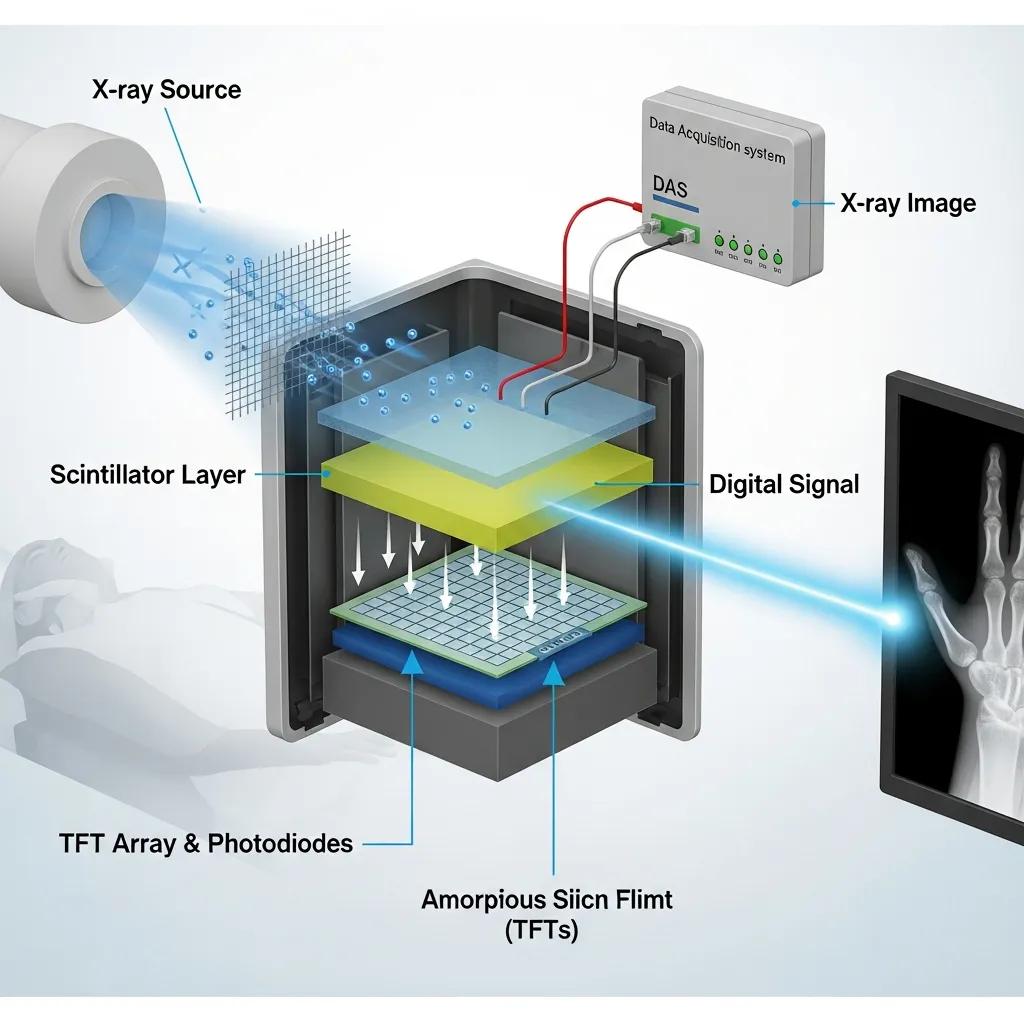
Digital X‑ray (digital radiography or DR) replaces film with electronic detectors that convert X‑ray photons into digital signals, allowing images to appear instantly and be processed by software. Detectors commonly use silicon or amorphous selenium arrays to capture transmitted radiation and produce a greyscale image that can be windowed, zoomed and enhanced in seconds. Because detectors are more photon‑efficient than film, exposures can often be reduced while maintaining diagnostic contrast. Images are stored in PACS for secure sharing with referrers. Faster turnaround, fewer repeats and immediate availability of images improve the patient experience and support multidisciplinary care — which naturally leads into when bedside or portable imaging is appropriate.
What are portable X‑ray systems and their applications?

Portable X‑ray systems are compact, mobile units that bring radiography to the patient instead of moving the patient to the radiology department. They’re commonly used at the bedside, in emergency departments, intensive care units and residential aged‑care facilities. By trading some detector size and fixed‑gantry geometry for mobility, portable units provide rapid assessment for conditions such as line placement, suspected pneumothorax and obvious fractures without patient transport. Modern portable units use digital detectors that deliver acceptable image quality for many indications, though fixed DR suites still offer higher spatial resolution for complex musculoskeletal or chest studies. Portability reduces logistical risk for unstable patients and complements fixed imaging services to balance image quality with access.
What are the key benefits of digital radiography compared to traditional X‑ray machines?
Digital radiography offers clear advantages over film‑screen radiography in dose management, speed and image quality — advantages that reduce repeat exposures and speed clinical decision‑making. Digital detectors use photons more efficiently, allowing lower exposure settings while keeping diagnostic contrast. Instant image availability shortens administrative turnaround and enables clinicians to act sooner. Software tools such as edge enhancement and noise reduction make abnormalities easier to see and support remote consultation via PACS. Together these benefits mean faster results, simpler archiving, fewer repeats and better information sharing between radiologists and referrers.
Before the direct comparison below, here are the main patient‑centred benefits of digital radiography:
- Lower radiation exposure: modern detectors often need less dose to produce diagnostic images.
- Quicker results: images are available immediately for review and reporting.
- Better image tools: contrast adjustments and zoom improve diagnostic visibility.
- Simpler sharing and storage: digital files integrate with PACS and teleradiology systems.
These advantages reduce delays and the need for repeat imaging, improving patient safety and clinical throughput. The table below summarises practical differences between digital radiography and traditional film‑based X‑ray.
The table compares key operational and patient‑centred attributes for quick reference.
This comparison shows how digital systems reduce cumulative exposure while improving access to images. As a result, many clinics have adopted digital radiography to improve outcomes and efficiency — a trend reflected in our local service offerings.
Life Medical Imaging Central Coast uses digital radiography across its services, supporting faster image turnaround and lower‑dose protocols. Patients and referrers can call to book or use our eReferral options to arrange imaging. This local adoption brings the clinical benefits described above to Central Coast clinicians and patients.
How does digital X‑ray reduce radiation exposure for patients?
Digital X‑ray reduces dose through more sensitive detectors, optimised exposure settings and image‑processing algorithms that enhance signal at lower photon counts. Modern detectors capture more useful information per X‑ray photon, enabling radiographers to use lower milliampere‑second settings while maintaining diagnostic contrast. Image‑processing and iterative reconstruction improve signal‑to‑noise ratios so diagnostic detail is preserved. Protocol‑driven exposures, dose monitoring and fewer repeats further limit cumulative exposure, which is especially important for repeat studies and vulnerable patients.
In what ways does digital radiography improve image quality and diagnosis speed?
Digital systems allow real‑time image review and adjustable windowing so clinicians can optimise contrast for bone, soft tissue or lung without extra exposures. Edge enhancement and magnification help detect subtle fractures and clarify pulmonary markings, improving diagnostic confidence. Faster transmission via PACS and integrated reporting shortens time‑to‑report and supports coordinated care, including remote referrals. Fewer retakes and smoother workflows mean clinicians receive actionable reports sooner, benefiting both acute care pathways and elective diagnostics.
How is X‑ray equipment used in different medical imaging services?
X‑ray technologies are matched to specific clinical services: DR is used for routine skeletal and chest radiographs; CT provides cross‑sectional detail for complex evaluation including cardiac CT and CT angiography; dental OPG captures panoramic jaw and dental anatomy; and DEXA measures bone density. Each modality answers different clinical questions — fracture vs cross‑sectional lesion characterisation vs dental assessment — and choices balance image detail against radiation and preparation requirements. Clinicians select the modality based on diagnostic need, access and dose considerations. The table below links equipment to common use cases and patient benefits.
The following table maps equipment types to typical clinical uses and expected patient benefits.
This mapping clarifies how each tool answers particular clinical questions and supports appropriate test selection. In practice, clinicians choose the modality that best balances diagnostic yield with patient comfort and safety.
At Life Medical Imaging Central Coast, our key services using these technologies include Digital X‑ray, Low Dose CT and Dental Imaging (OPG). We offer online appointment booking and eReferral to help referrers and patients arrange the most suitable test. Local availability reduces delays and supports continuity of care for Central Coast patients.
What role does X‑ray equipment play in low dose CT scans?
Computed tomography uses X‑rays taken from multiple angles to reconstruct cross‑sectional and volumetric images. Low‑dose CT (LDCT) protocols reduce tube current, use rapid rotation and apply iterative reconstruction to lower dose while preserving diagnostic information. LDCT is useful for chest imaging, lung nodule follow‑up and selected cardiac assessments where detail is needed without excessive exposure. Iterative reconstruction and modern detector arrays compensate for lower signal by reducing noise and artefact, maintaining diagnostic confidence. The optimal balance between dose and image fidelity is achieved by tailoring protocols to the clinical question — standard practice in modern CT services.
How are dental X‑ray machines utilised in dental imaging?
Dental imaging includes intraoral bitewing and periapical sensors for high‑resolution tooth‑level views and panoramic OPG units for a complete view of the mandible, maxilla and dentition. An OPG produces a single curved‑plane panoramic image that assists with orthodontic planning, implant assessment and detection of jaw pathology; intraoral digital sensors provide the fine detail needed for caries and root assessment at low dose. Digital dental sensors speed up acquisition and integrate with practice software for rapid diagnosis and treatment planning. Patients typically experience brief exposures and minimal discomfort while staff ensure proper positioning and removal of metallic objects to optimise image quality.
How should patients prepare for X‑ray imaging procedures using advanced equipment?
Preparing for X‑ray, CT or dental imaging is simple when you follow modality‑specific guidance. Typical preparation includes removing jewellery and metal objects, wearing comfortable clothing, advising staff if you’re pregnant and following any fasting or hydration instructions when contrast is planned for CT. Clear pre‑scan instructions reduce delays and the chance of repeat imaging. Staff will provide shielding where appropriate and explain each step to put you at ease. The checklist below summarises essential preparation steps for most X‑ray and CT appointments.
Follow this numbered checklist before attending an imaging appointment to help ensure a smooth visit:
- Tell staff if you are pregnant or suspect you may be pregnant so we can arrange an alternative pathway or postpone if needed.
- Remove jewellery, removable dental appliances and other metal that could cause image artefact.
- Wear loose, comfortable clothing — you may be asked to change into a gown for some studies.
- Follow fasting instructions if a contrast CT is planned and bring a list of current medications.
- Bring your referral, any prior imaging and a photo ID to speed up registration.
These practical steps minimise delays and support image quality. Staff will confirm any additional modality‑specific requirements when you arrive and guide you through the process.
What should patients expect during a digital X‑ray appointment?
A typical digital X‑ray appointment begins with registration, confirmation of the clinical reason and a short safety screen that focuses on pregnancy and previous surgeries. The radiographer will position you on the table or against a bucky detector and may provide a lead apron where indicated. Exposures are quick and painless, usually just seconds per view. Images appear instantly and the radiographer will check them on the spot to avoid unnecessary repeats; images and a report are then sent to the referring clinician for interpretation. This straightforward workflow helps set expectations for timing and result delivery.
Are there special considerations for low dose CT or dental X‑ray scans?
Low‑dose CT and dental imaging have specific preparation and safety checks to protect patients and ensure diagnostic quality. For CT with intravenous contrast, fasting and renal function checks may be required — these will be communicated in advance. Low‑dose protocols adjust scanner settings to meet the clinical need with minimal exposure. Dental imaging often requires removal of metal and correct bite positioning to prevent repeats; panoramic OPGs are quick and low dose. Let staff know about implants, prostheses or claustrophobia so we can provide appropriate alternatives or accommodations.
Life Medical Imaging Central Coast accepts referrals and provides eReferral and online booking to clarify preparation before arrival. Bringing your referral and any prior imaging helps streamline your appointment and supports accurate reporting.
Why choose Life Medical Imaging Central Coast for your X‑ray equipment services?
Life Medical Imaging Central Coast is a NATA‑accredited independent radiology provider serving multiple sites across the Central Coast. We offer a range of X‑ray‑based services with patient‑centred access, supported by experienced staff and modern equipment. Our service notes highlight “Ultra‑low Dose, High Definition” capabilities, online booking and eReferral options — features that help referrers and patients access timely, high‑quality imaging without unnecessary delay. These attributes align with best practice for safety, clarity and convenience in diagnostic imaging.
This summary shows how available technologies translate into clinical impact, helping referrers and patients access high‑quality imaging close to home.
What advanced X‑ray technologies are available at Life Medical Imaging?
Life Medical Imaging Central Coast lists core X‑ray capabilities including digital X‑ray systems, low‑dose CT described as “Ultra‑low Dose, High Definition”, and dental OPG for panoramic dental evaluation. These services support modern imaging workflows that prioritise image clarity and dose reduction. Multiple clinic locations and eReferral/online booking make it easier for referrers to coordinate access and for patients to attend the right service when they need it.
How does Life Medical Imaging ensure patient comfort and safety?
Our NATA accreditation reflects adherence to recognised quality standards. We combine patient‑centred care from qualified staff with modern facilities and dose‑aware imaging protocols. Multiple clinic locations and online booking reduce travel and administrative friction, while staff training in low‑dose practice and up‑to‑date protocols supports safety and comfort. Together, these measures give referrers and patients confidence in the services we provide.
What are common questions about X‑ray equipment and medical imaging?
Clinicians and patients often ask how radiography differs from fluoroscopy, what role AI plays and how low‑dose protocols affect care. The short Q&A below gives direct, evidence‑framed answers to common queries and highlights trends that influence test selection and reporting.
- What is the difference between conventional radiography and fluoroscopy? Conventional radiography produces static 2D images useful for fractures and chest films; fluoroscopy provides continuous real‑time imaging for procedures such as contrast studies and interventional guidance.
- How do innovations like AI and low‑dose protocols shape X‑ray equipment? AI helps triage studies and flag potential abnormalities while low‑dose protocols and advanced reconstruction preserve diagnostic quality with reduced exposure.
- Who should I contact to arrange imaging or discuss protocol suitability? Referrers should use our eReferral channels and patients can call the clinic to book appointments or ask questions about preparation and suitability.
These concise answers give quick guidance and show how equipment choice maps to clinical needs. The following sections expand on the radiography vs fluoroscopy difference and current innovation trends.
What is the difference between conventional radiography and fluoroscopy?
Conventional radiography captures single or a few static images ideal for assessing fractures, chest disease or abdominal gas patterns — quick diagnostics with minimal setup. Fluoroscopy provides continuous dynamic imaging for procedures such as contrast swallow studies, catheter placement and interventional guidance where live visual feedback is needed. Because fluoroscopy can involve longer exposure times, stricter dose‑management measures and additional shielding are used, and procedural staff are trained to minimise cumulative exposure. The modality chosen depends on whether the clinical question needs static diagnostic images or continuous, real‑time visualisation for assessment or treatment.
How are innovations like AI and low‑dose protocols shaping X‑ray equipment?
AI and algorithmic reconstruction are changing how images are acquired, processed and triaged. AI can prioritise studies that appear abnormal, assist with measurements and support radiologist workflow, though clinical oversight remains essential. Low‑dose acquisition strategies combined with iterative reconstruction and improved detectors reduce radiation while maintaining or enhancing diagnostic detail, enabling safer repeat imaging and more effective screening. Together these advances boost diagnostic throughput, support remote reporting and reduce dose burden — practical benefits many clinics adopt to improve patient care and operational efficiency.
Frequently asked questions
What are the safety measures in place for X‑ray imaging?
Safety measures include use of lead aprons where appropriate, careful positioning to minimise exposure and adherence to low‑dose protocols. Radiographers follow strict guidelines to ensure patient safety, including verifying pregnancy status and using the lowest effective dose. Modern digital systems also allow real‑time monitoring and exposure adjustments, further supporting safe, high‑quality imaging.
How often should patients undergo X‑ray imaging?
Frequency depends on individual health needs and the clinical indication. Some chronic conditions require periodic imaging for monitoring, while acute issues may need one‑off scans. Your healthcare provider will recommend timing and frequency based on your medical history, symptoms and the diagnostic value of the imaging.
What advancements are being made in X‑ray technology?
Key advancements include ultra‑low dose imaging, improved detector sensitivity and the integration of AI for image analysis and workflow support. These developments enhance image quality while reducing radiation exposure. Improved software for image processing also helps visualise complex anatomy more clearly, aiding faster and more accurate clinical decisions.
Can X‑ray imaging be performed on pregnant patients?
X‑ray imaging may be performed in pregnancy when clinically necessary, but it requires careful consideration and precautions. Radiographers will evaluate the need for imaging and, where possible, offer alternatives. If an X‑ray is essential, protective measures such as lead shielding are used to minimise fetal exposure. Always inform staff if you are pregnant or think you might be.
What should patients do if they have metal implants before an X‑ray?
Tell your radiographer or referrer about any metal implants before the procedure. Most modern X‑ray systems can accommodate implants, but certain studies may need adjustments to technique or positioning. The radiographer will advise on precautions to ensure image quality and diagnostic accuracy.
How do I know if I need an X‑ray or another imaging modality?
Your healthcare provider will recommend the most suitable modality after reviewing your symptoms and medical history. X‑rays are often appropriate for fractures and basic assessments, while CT or MRI may be better for complex or cross‑sectional evaluation. Your referrer will guide you to the best test for your situation.
What is the role of AI in modern X‑ray imaging?
AI supports radiology by improving workflow efficiency, prioritising urgent studies, detecting potential abnormalities and assisting with measurements. It can also enhance image quality through advanced processing. AI is a tool to assist radiologists — clinical review and oversight remain vital to ensure accurate interpretation and patient safety.
Conclusion
Knowing the types and benefits of X‑ray equipment helps clinicians and patients make informed decisions and improves diagnostic care. Modern technologies such as digital radiography and low‑dose CT enable high‑quality imaging while minimising radiation exposure. For reliable local imaging, Life Medical Imaging Central Coast provides a broad range of X‑ray services delivered with a focus on safety, clarity and patient comfort. Visit our services page or contact the clinic to arrange imaging tailored to your needs.

