Advanced diagnostic imaging: innovations, benefits and next steps
Advanced diagnostic imaging brings together several technologies that help detect disease earlier, guide treatment and reduce risk by improving image clarity and lowering radiation where possible. This article walks through innovations — ultra‑low dose CT, high‑definition reconstruction, 3D/4D ultrasound, AI‑assisted image processing and modern digital X‑ray — and explains, in plain terms, what each does, how it helps clinicians and patients, and what to expect at your appointment. We also cover advances in cardiac CT angiography, emerging whole‑body techniques and the clinic‑level quality systems that protect patients and support reliable reporting. Throughout, the content balances technical accuracy for referrers with clear, reassuring language for patients and points to local service availability and booking options where relevant.
What is ultra‑low dose CT technology and how does it improve patient safety?
Ultra‑low dose CT refers to combined hardware and software improvements that produce diagnostic images while significantly reducing ionising radiation compared with older CT techniques. The approach pairs more sensitive detectors and faster acquisition with optimised scan protocols tailored to the clinical question, plus advanced reconstruction methods — including iterative techniques and AI‑based denoising — to maintain high‑definition detail at lower tube currents. For patients, the lower dose reduces stochastic risk while preserving the spatial and contrast resolution clinicians need for confident diagnosis; this is especially important for people who require repeat surveillance scans. Knowing how these elements work together helps explain why many modern CT systems can deliver excellent image quality at a much lower dose, supporting safer imaging pathways for a wide range of patients.
Life Medical Imaging Central Coast offers ultra‑low dose, high‑definition CT scanning as part of our diagnostic services. For more information about this test or to arrange an appointment, please contact our clinic or speak with your referrer.
Advanced Diagnostic Imaging: Innovations, Benefits, and Future Trends
This overview describes how advances such as ultra‑low dose CT, high‑definition reconstruction, 3D/4D ultrasound, AI‑assisted image processing and modern digital X‑ray systems lead to clearer diagnoses and safer patient pathways. It explains each technology at a practical level, outlines benefits for patients and referring clinicians, and sets expectations for appointments and local service availability.
Feasibility of an ultra‑low dose contrast media protocol for coronary CT angiography, 2022
How does ultra‑low dose CT reduce radiation exposure?
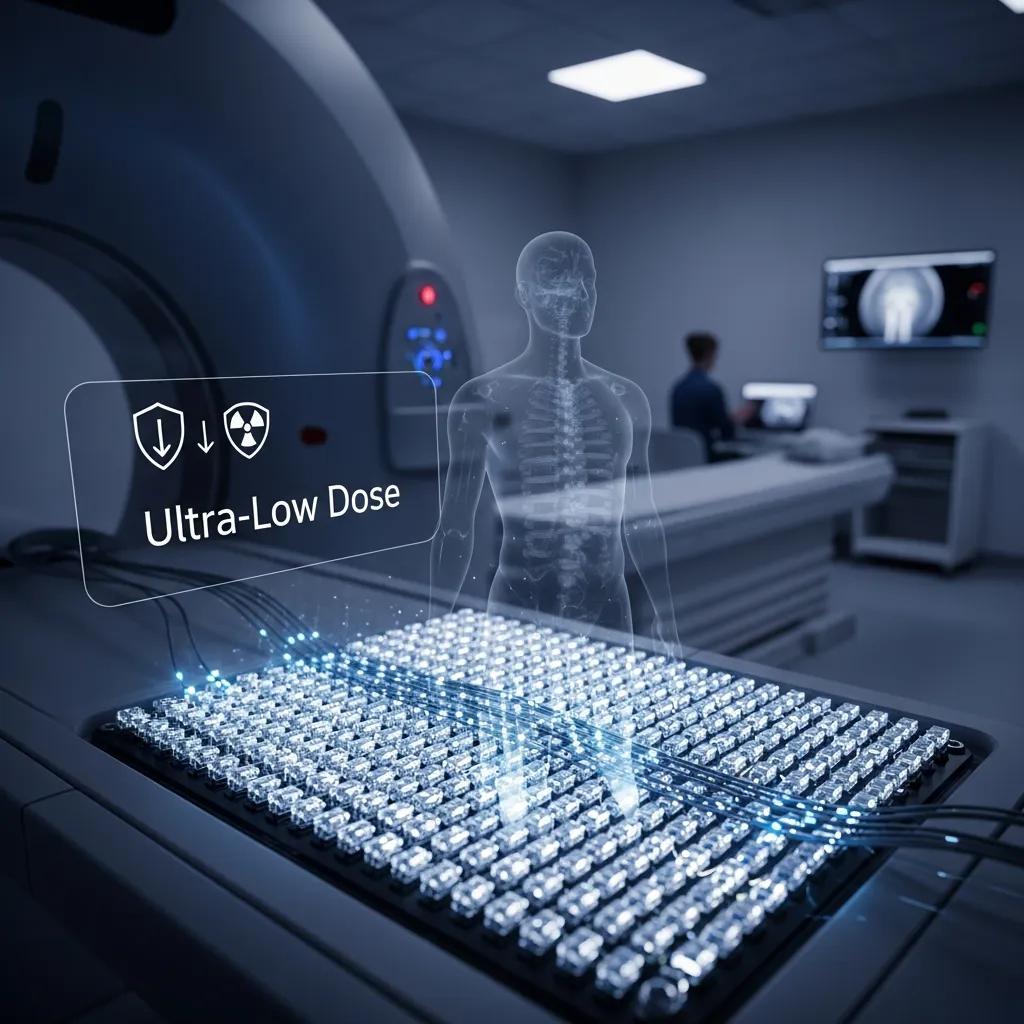
Ultra‑low dose CT lowers exposure by combining more sensitive detectors, smarter acquisition and advanced post‑processing to recover image quality from fewer X‑ray photons. Modern detectors capture a stronger signal per photon and cut electronic noise, enabling scans at lower tube currents while keeping contrast. Iterative reconstruction and AI denoising suppress noise and sharpen edges in the final image. Protocol optimisation — adjusting scan length, kVp and acquisition mode for patient size and the specific clinical question — further reduces unnecessary exposure and helps avoid repeat imaging. These layered strategies produce meaningful dose reductions without sacrificing the diagnostic detail clinicians rely on.
What are the clinical benefits of high‑definition CT scans?
High‑definition CT gives clearer characterisation of small lesions, more precise delineation of vascular anatomy and better visualisation of complex structures — all of which directly influence clinical decisions. For example, improved spatial resolution helps distinguish calcified from non‑calcified plaque in coronary imaging, enhances lung nodule assessment and refines surgical planning for abdominal or oncological procedures. Greater lesion conspicuity can reduce the need for extra imaging or invasive tests by increasing confidence in initial reports, shortening diagnostic pathways and accelerating treatment. For referring clinicians and patients alike, the result is faster, more accurate diagnosis with fewer follow‑ups and clearer guidance for therapy.
Different detector technologies and reconstruction methods affect resolution, dose and clinical usefulness in measurable ways. The table below summarises common detector/reconstruction combinations and their typical clinical uses to help with referral decisions.
This comparison demonstrates how detector sensitivity and reconstruction choices affect image fidelity and achievable radiation dose, helping clinicians match modality to clinical need.
Photon‑Counting Detector CT: Technical Advancements and Imaging Benefits
Compared with traditional energy‑integrating detectors, photon‑counting detectors offer finer spatial resolution, a higher contrast‑to‑noise ratio, reduced electronic noise, better dose efficiency and routine multi‑energy imaging. This review introduces PCD‑CT technology, summarises reported imaging benefits across preclinical and clinical systems, and discusses current limitations and potential improvements.
The technical development of photon‑counting detector CT, CH McCollough, 2023
How does 3D/4D ultrasound technology enhance obstetric and diagnostic imaging?
3D and 4D ultrasound capture volumetric anatomy and real‑time motion, adding depth and context beyond standard 2D views and improving both diagnostic accuracy and the patient experience. Volumetric acquisition enables multiplanar reformats and surface rendering that clarify fetal anatomy, facial structures and complex musculoskeletal relationships, while 4D adds temporal information useful for assessing motion and function. Because ultrasound uses no ionising radiation, these modalities are safe for antenatal imaging and repeated assessments, making them valuable in pregnancy care and other specialties. Clearer visualisation supports earlier detection, better counselling and improved planning when intervention is required.
We provide 3D/4D obstetric imaging at Life Medical Imaging Central Coast for antenatal assessment and parental reassurance. Contact us for service details or to book an appointment.
What are the key features of 3D/4D ultrasound imaging?
3D ultrasound captures volumetric datasets that can be reformatted into multiplanar views and rendered to show surface anatomy or internal structures with depth perception. Rendering modes — surface, transparent and colour mapping — help clinicians evaluate fetal face, limbs and structural anatomy alongside 2D screening; 4D adds real‑time motion to show functions such as fetal breathing or cardiac activity. Post‑processing and image sharing let clinicians review and measure structures offline, improving reproducibility and multidisciplinary discussion. These capabilities make volumetric ultrasound especially useful when anomalies are suspected or a detailed anatomical survey is needed.
How do 3D/4D ultrasound benefits impact pregnancy care?

3D/4D imaging improves detection of structural anomalies and helps with parental counselling by presenting anatomy in a clear, intuitive way. Targeted volumetric scans can clarify findings from 2D screening, guide referral to specialist fetal medicine and support multidisciplinary planning for delivery or postnatal care. Because ultrasound involves no ionising radiation, it is safe for serial assessments during pregnancy — useful for monitoring growth, function and structural change over time. Combined, better diagnostic precision and clearer communication reduce uncertainty for parents and clinicians and enable timely, evidence‑based care.
To guide referrals and parental expectations, the applications of 2D, 3D and 4D ultrasound can be summarised as follows.
- 2D Ultrasound: Standard structural survey and screening in early and mid‑pregnancy.
- 3D Ultrasound: Detailed anatomical assessment and surface rendering to clarify suspected anomalies.
- 4D Ultrasound: Real‑time functional assessment and enhanced visualisation for counselling.
AI‑Enhanced 3D/4D Ultrasound for Fetal Analysis
Artificial intelligence is increasingly applied to 3D/4D ultrasound, improving the analysis of complex volumetric data and supporting more consistent, efficient interpretation. Machine learning tools can assist with biometric measurements and facial profile assessment, helping clinicians make informed prenatal decisions and enhancing the quality of prenatal care.
The utilization of artificial intelligence in enhancing 3D/4D ultrasound analysis of fetal facial profiles, MA Bachnas, 2024
How is artificial intelligence transforming medical imaging diagnostics?
AI in medical imaging covers algorithms that help with image reconstruction, automated detection and measurement, triage and structured reporting — all aimed at improving accuracy and workflow efficiency. AI can denoise low‑dose acquisitions, speed up reconstruction and generate quantitative metrics (for example, calcium scoring or volumetry) that support reproducible assessment. In triage roles, AI flags urgent findings for faster review, reducing time‑to‑report for critical cases and improving patient safety. While regulation and validation shape adoption, evidence through 2024–2025 shows measurable gains in sensitivity, reporting speed and inter‑reader consistency when AI tools are integrated responsibly.
What roles does AI play in improving scan accuracy and reporting?
AI enhances scan accuracy by improving image quality through reconstruction and denoising, detecting subtle patterns that can be missed by the eye, and standardising measurements to reduce variability. Examples include automated lung nodule detection that helps prioritise suspicious cases and AI‑assisted calcium scoring that provides objective cardiac risk metrics. Structured reporting templates populated with AI‑derived measurements streamline communication to referrers and support consistent follow‑up advice. These tools augment radiologist expertise, letting clinicians focus on complex interpretation while routine quantification and alerting are handled efficiently.
How is AI being adopted in CT and ultrasound imaging?
In CT, adoption has concentrated on reconstruction acceleration, denoising for dose reduction and computer‑aided detection for organs such as lung and liver. In ultrasound, AI focuses on automated biometric measurements and image‑quality enhancement. Vendors now offer integrated AI modules while some research tools remain in trial phases; regulatory approval and clinical validation determine which tools move into routine practice. Practical barriers include integration with reporting systems, validation across diverse patient groups and demonstrating workflow return on investment. The overall trend is toward hybrid workflows where AI supports both technical image enhancement and clinical decision support.
AI‑driven tools complement hardware advances and help translate technical improvements into reliable clinical benefit, leading naturally to innovations in cardiac CT and vascular imaging.
What are the latest innovations in cardiac CT and CT angiography technology?
Cardiac CT and CT angiography (CCTA) have benefited from faster detectors, ECG‑gating techniques, high‑definition reconstruction and AI denoising, all of which reduce motion artefact and achievable radiation dose. These advances enable non‑invasive visualisation of coronary anatomy, plaque characterisation and functional surrogates that help diagnose coronary artery disease and plan interventions. Prospective gating, high temporal resolution acquisition and advanced reconstruction preserve image quality even at ultra‑low dose settings, expanding the patients for whom non‑invasive coronary imaging is a useful option. Clinicians use these tools to exclude significant obstructive disease in low‑to‑intermediate risk patients and to inform downstream management efficiently.
How does cardiac CT angiography improve heart disease diagnosis?
CCTA non‑invasively maps the coronary arteries with high sensitivity for clinically significant stenosis, allowing rapid exclusion of obstructive coronary disease in many patients presenting with chest pain. The test also characterises plaque composition and distribution, adding prognostic information beyond lumen narrowing and influencing medical therapy and revascularisation decisions. For pre‑procedural planning it provides three‑dimensional anatomy useful for structural interventions and bypass graft assessment. As a result, CCTA can shorten diagnostic pathways and reduce unnecessary invasive angiography when patients are appropriately selected.
What technological features enable ultra‑low dose cardiac CT scans?
Ultra‑low dose cardiac CT uses prospective ECG‑gating to limit X‑ray exposure to narrow cardiac phases, high temporal resolution detectors to reduce motion blur, and iterative or AI‑enhanced reconstruction to recover image detail from a smaller signal. Prospective gating confines exposure to targeted cardiac windows rather than continuous scanning, while modern detectors capture clearer signals at lower currents. AI denoising permits lower tube current settings without compromising diagnostic detail, and protocol tailoring limits scan coverage to the clinical question. Together these elements let clinicians obtain clinically useful cardiac images with far lower radiation than older techniques.
These combined features enable clinicians to obtain high‑quality cardiac images with substantially lower radiation than older CT technologies.
Key clinical advantages of CCTA include:
- Non‑invasive evaluation of coronary anatomy and stenosis.
- Plaque characterisation to inform prognosis and therapy.
- Accurate pre‑procedural mapping for interventions and bypass assessment.
How do digital X‑ray and emerging imaging modalities enhance diagnostic access?
Modern digital X‑ray systems and portable radiography increase access to imaging by enabling rapid acquisition, immediate review and bedside studies that reduce patient movement and logistical delays. Contemporary digital detectors deliver quality images at lower dose than older film‑screen systems and integrate directly with reporting workflows. Emerging modalities such as total‑body PET offer much higher sensitivity and faster whole‑body functional assessment, opening possibilities for earlier detection and more precise longitudinal monitoring in oncology and inflammatory disease. Together, these technologies shorten diagnostic timelines, improve patient comfort and broaden the settings where definitive imaging can take place.
What are the advantages of portable and digital X‑ray systems?
Portable and digital X‑ray systems make imaging available at the bedside in emergency departments, inpatient wards and aged‑care settings, reducing the need to move vulnerable patients and speeding decision‑making. Digital workflows provide instant image review, faster reporting turnaround and easier comparison with prior studies when integrated with PACS and reporting systems. Many indications — for example chest radiography to assess consolidation or line and tube position — can be reliably addressed with portable units that meet the diagnostic need while limiting transport burdens. For patients this means quicker answers, less disruption and often a more comfortable experience.
What is total‑body PET and how does it advance diagnostic imaging?
Total‑body PET is an emerging nuclear medicine platform that images the entire body simultaneously with much higher sensitivity than conventional PET scanners, allowing faster scans, lower radiotracer doses or both. The improved sensitivity supports whole‑body kinetic studies and more precise quantitative measures that enhance cancer staging, detect early systemic inflammation and monitor treatment response across multiple sites. Availability is still limited as the technology spreads, but early clinical and research findings point to substantial potential to change how whole‑body functional imaging informs diagnosis and therapy. Clear information about availability and clinical utility helps referrers plan the right diagnostic strategy.
To compare modalities succinctly, the table below summarises portability, sensitivity and typical access benefits.
This comparison highlights how choice of modality affects patient pathways and practical access to decisive imaging.
How does Life Medical Imaging ensure patient safety and quality with advanced technology?
Life Medical Imaging Central Coast combines modern equipment, specialist staff and robust quality systems to keep imaging accurate, reproducible and focused on patient safety. We operate within recognised accreditation frameworks, follow dose‑minimisation protocols, maintain ongoing staff training and perform equipment quality assurance to ensure consistent performance across modalities. Technology such as iterative reconstruction, gating and structured reporting supports consistency in interpretation, and clear referral and preparation guidance helps patients arrive ready for their scan. Together, these organisational and technical measures make imaging safe, timely and actionable for clinical care.
Life Medical Imaging Central Coast is an independent, NATA‑accredited radiology clinic offering a broad range of diagnostic imaging services across the Central Coast. For more information about our services or to book an appointment, please contact the clinic.
What measures minimise radiation exposure in diagnostic imaging?
We reduce radiation exposure through protocol tailoring, careful modality selection, shielding when appropriate and use of equipment features such as prospective gating and advanced reconstruction. Staff training ensures each scan is justified for the clinical question and optimised for patient size and condition, while dose indices are monitored to detect deviations and prompt corrective action. Patients can help by bringing prior imaging or a clear referral indication so scans are planned to avoid unnecessary repeats. These steps reduce cumulative exposure and ensure the diagnostic benefits outweigh any risk.
How does technology support accurate and reliable imaging results?
Hardware, software and workflow measures work together to support diagnostic reliability: modern detectors and reconstruction improve raw image data, AI and post‑processing produce quantitative measures and structured reporting ensures clear communication. Quality assurance processes, double‑reading for selected complex studies and regular calibration maintain performance over time, while digital archiving and teleradiology enable timely review and multidisciplinary input. These systems deliver reproducible, traceable reports clinicians can rely on for management decisions. Patients benefit from faster, clearer results and well‑defined next steps after imaging.
Our services reflect these quality priorities and support local referrers and patients.
- General and specialised CT (including cardiac CT and CT angiography).
- Digital X‑ray, ultrasound across multiple specialties, and bone densitometry.
- Interventional procedures and therapeutic injections such as platelet‑rich plasma where clinically indicated.
Life Medical Imaging Central Coast provides comprehensive diagnostic imaging and patient‑centred care across locations including Bateau Bay, Killarney Vale, Umina Beach and Erina. Contact us for service details or to book an appointment.
Frequently Asked Questions
What is the role of AI in enhancing patient outcomes in diagnostic imaging?
AI supports better patient outcomes by improving image quality, speeding detection of important findings and standardising measurements. It can help highlight urgent cases, automate routine measurements and reduce variability between readers, which shortens reporting times and supports timely treatment. When used alongside clinician review and robust validation, AI helps deliver faster, more consistent care.
How do modern imaging technologies impact the cost of healthcare?
Advanced imaging can reduce downstream costs by improving diagnostic accuracy, cutting the need for invasive tests and avoiding repeat scans. Bedside imaging and faster workflows reduce transport and hospital stay costs. While equipment investment is significant, better diagnosis and more efficient care pathways often lead to long‑term savings and improved patient outcomes.
What should patients expect during their imaging appointments?
Patients should expect a clear explanation of the procedure, guidance on how to prepare and support from our staff throughout the visit. Depending on the test, you may be asked to remain still or follow simple breathing instructions; most scans are quick. After the scan, you’ll be told when to expect results and any recommended next steps.
Are there any risks associated with advanced imaging technologies?
All imaging carries some risk — for example, CT uses ionising radiation — but modern techniques like ultra‑low dose CT significantly reduce exposure. Risks are weighed against the diagnostic benefits, and staff take steps to minimise exposure and discomfort. If you have concerns, speak with your referrer or our team so we can explain safety measures and alternatives.
How does Life Medical Imaging ensure the quality of its imaging services?
Quality is maintained through accredited equipment, regular maintenance and calibration, ongoing staff training and adherence to dose‑minimisation and reporting standards. We follow established quality assurance processes and participate in accreditation frameworks to ensure every procedure meets clinical and safety expectations.
What advancements are being made in the field of ultrasound imaging?
Advances include 3D and 4D volumetric imaging, improved transducer design and AI‑assisted measurement and image enhancement. These developments sharpen diagnostic capability in obstetrics and other specialties, speed workflows and improve consistency of reporting, all of which support better clinical decision‑making.
Conclusion
Modern diagnostic imaging — from ultra‑low dose CT to 3D/4D ultrasound and AI‑assisted tools — improves diagnostic clarity and patient safety while helping clinicians make faster, better‑informed decisions. Life Medical Imaging Central Coast offers access to these technologies with patient‑centred care and robust quality systems. To learn more about our services or to book an appointment, contact your local clinic today.

