MRI Guide — Understanding Scans, Costs, Safety and How to Prepare
Magnetic Resonance Imaging (MRI) is a non-invasive imaging method that uses strong magnetic fields and radiofrequency pulses to produce detailed images of soft tissues, organs and the nervous system. This guide explains how MRI works, the common scan types and their clinical uses, and practical advice on preparation, safety and what to expect before, during and after a scan. We also address common patient questions about costs, when MRI is preferred over CT, and how implants or pregnancy can affect suitability. You’ll find clear comparisons, safety and preparation checklists, and tables summarising typical cost ranges and modality differences to help you make informed choices. Where relevant, the guide points to alternatives such as CT and ultrasound and explains how a local Central Coast provider can help with referrals and bookings. Read on for straightforward, clinically relevant information so you can approach imaging with confidence.
What Is an MRI Machine and How Does It Work?
An MRI machine produces detailed internal images by aligning hydrogen protons in the body with a powerful magnetic field, then briefly disturbing that alignment with radiofrequency pulses and recording the signals that follow. The combination of magnetism, RF excitation and signal processing creates contrast between tissues by using differences in relaxation times (T1 and T2), which is why MRI is particularly good at showing soft-tissue detail. Because MRI doesn’t use ionising radiation, it’s often preferred for neurological, musculoskeletal and other soft-tissue assessments. The following sections explain how magnetic fields and radio waves create images and why MRI avoids ionising radiation — key background for the safety and preparation advice that follows.
How Do Magnetic Fields and Radio Waves Create MRI Images?
Hydrogen protons in water molecules align with the scanner’s main magnetic field. A targeted radiofrequency (RF) pulse tips this alignment; when the protons relax back they emit RF signals picked up by coils and processed into images. Contrast arises from how quickly protons return to equilibrium (T1 and T2 relaxation), and choosing specific sequences emphasises particular tissue differences for diagnosis. Surface RF coils placed near the body act as sensitive receivers to boost signal-to-noise and resolution, while gradient coils spatially encode signals to form slices. That signal chain explains why coil selection, field strength and sequence choice directly affect image detail and scan time.
Why Does MRI Use No Ionising Radiation?
MRI works in the radiofrequency part of the electromagnetic spectrum, which deposits energy without ionising atoms or breaking chemical bonds — unlike X-rays used in CT. Because MRI relies on magnetic resonance rather than ionising photons, it does not contribute to cumulative radiation exposure. That makes MRI a safer option for repeat imaging and for younger patients when clinically appropriate. This radiation-free advantage is important in areas such as neurology and paediatrics, though other safety checks (for example, implant compatibility) remain essential.
What Are the Different Types of MRI Scans and Their Uses?
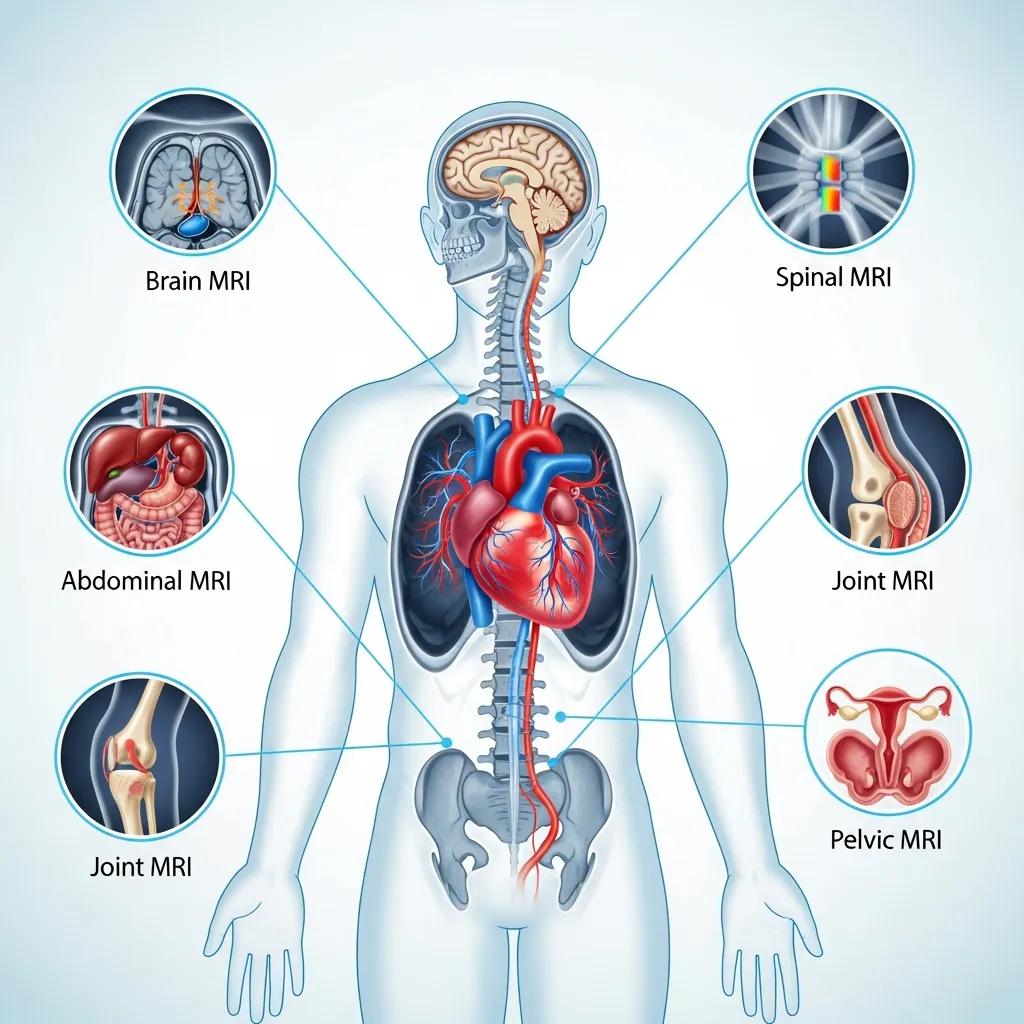
MRI covers a range of tailored studies including brain MRI, spinal MRI, musculoskeletal (joint) MRI, cardiac MRI, MR angiography and whole-body MRI for staging or specific screening in selected cases. Each study uses dedicated coils and sequences to highlight relevant pathology — for example, diffusion-weighted imaging for acute brain ischaemia, T2-weighted scans for spinal cord lesions, and cine sequences for cardiac function. Advanced techniques such as functional MRI map brain activation, while MR angiography visualises blood vessels often without iodinated contrast. The table below summarises common MRI subtypes, typical indications and how contrast is usually used.
Which Body Parts and Conditions Can MRI Diagnose?
MRI is the preferred test for many brain and spinal conditions including tumours, multiple sclerosis, infection and acute ischaemia — where diffusion-weighted imaging is essential. It also offers superior soft-tissue contrast for joint problems such as ligament tears, cartilage damage and occult fractures, and it’s valuable for assessing cardiac function and myocardial tissue. Abdominal MRI helps characterise liver lesions and pelvic pathology, while whole-body protocols can assist in cancer staging and conditions like myeloma. These strengths explain why clinicians select MRI when detailed soft-tissue resolution or repeat imaging without radiation is important.
What Are Open MRI Machines and When Are They Recommended?
Open MRI systems have a less confining design or wider bore, which reduces claustrophobia and can accommodate larger patients. They are often lower field-strength systems, which may reduce resolution for some indications. Open scanners are a good option for patients with anxiety, severe claustrophobia or body habitus that prevents safe positioning in a tunnel scanner; focused, faster sequences help reduce motion artefact. For the highest-resolution studies — for example, subtle neurological detail — a higher-field closed-bore scanner (1.5T or 3T) is usually preferred. If comfort is the priority, discuss the potential trade-offs in image quality with your referrer to ensure the chosen scanner meets the diagnostic need.
How Much Does an MRI Scan Cost in the UK?
Private MRI costs in the UK vary by region, scanner type and study complexity. Typical ranges are: single-area non-contrast scans around £250–£450; contrast-enhanced or multi-region studies from about £400–£900. Prices reflect scanner field strength, use of contrast, sequence complexity, subspecialist reporting and local facility fees. Urgent appointments or private reports may add to the cost. The table below gives common private MRI types with approximate UK price ranges and typical scan times to help with planning.
What Factors Influence MRI Scan Prices?
Several factors affect MRI pricing: the scanner’s field strength and technology (1.5T vs 3T), whether gadolinium is required, the number and complexity of sequences, subspecialist radiologist reporting and local operating costs. Extra charges can come from sedation or anaesthesia for anxious or paediatric patients, urgent or out-of-hours appointments, and image copy or transfer services. Always ask for an itemised estimate and check if private insurance or your referrer covers part of the fee. Knowing these cost drivers helps you compare options and ask the right questions when booking privately.
Are There Payment or Insurance Options for MRI Scans?
Private MRI scans are usually paid for either out-of-pocket or via private medical insurance, depending on policy terms. Many insurers require pre-authorisation and a clinical referral before approving funding. Imaging centres can provide written estimates and invoices for claims; check whether subspecialist reporting is included. If MRI isn’t available locally, some providers arrange referrals or offer guidance on alternatives. Contact your insurer early and obtain pre-authorisation where required to avoid unexpected costs.
What Are MRI Safety Guidelines and Contraindications?

Is MRI safe? For most people, yes — MRI is generally safe because it uses non-ionising radiofrequency energy. However, the strong magnetic field can interact with metallic implants, electronic devices and some foreign bodies, so thorough safety screening is essential. Absolute contraindications include certain non-MR-conditional cardiac pacemakers and particular metallic fragments in sensitive areas; relative contraindications include severe claustrophobia, some implanted devices that need specialist review, and impaired renal function when contrast is being considered. The list below highlights common contraindications and screening steps taken before scanning.
- Non-MR-conditional cardiac pacemakers or certain implanted electronic devices require specialist review.
- Recent metallic fragments (for example ocular or intracranial) may preclude MRI unless proven safe.
- Severe claustrophobia, anxiety or inability to lie still may mean open MRI or sedation is needed.
- Impaired renal function is assessed before administering gadolinium-based contrast.
Patient safety is our priority — careful screening and clear documentation help ensure MRI can be performed safely when appropriate.
MRI Safety and Compatibility of Implants
Issues such as injuries from implant–MRI interactions are discussed in the literature and inform current screening practices.
MRI safety and compatibility of implants and medical devices, TO Woods, 2003
Can You Have an MRI with Metal Implants or Pacemakers?
Many orthopaedic implants (for example joint replacements) are made from non-ferromagnetic materials and are safe in MRI. Older pacemakers and some neurostimulators can be unsafe unless they are explicitly labelled MR-conditional and managed under device-specific protocols. Safe MRI with implanted devices requires documentation of device make and model, conditionality information, and coordination between the radiology and device teams — sometimes including device programming or monitoring. Bring implant cards, operation notes or implant stickers to your appointment and tell the imaging team about any prior surgeries; this helps determine compatibility and plan any necessary precautions so MRI can often proceed safely.
What Are the Risks of Contrast Dye and Pregnancy Considerations?
Gadolinium-based contrast agents improve tissue characterisation but carry small risks such as rare allergic reactions and, in severe renal impairment, a low risk of nephrogenic systemic fibrosis. Current guidance recommends cautious use and renal function assessment where indicated. During pregnancy, non-contrast MRI is generally considered safe when clinically necessary, particularly after the first trimester; gadolinium is avoided unless absolutely essential because of potential fetal exposure. Decisions about contrast are made in consultation with the referrer, weighing clinical need, allergic history and renal function to minimise risk.
How Should You Prepare for an MRI Scan?
Good preparation reduces delays and improves image quality. Bring your referral and any implant documentation, remove metal objects and jewellery, wear loose clothing without metal fastenings and follow fasting instructions only if contrast or sedation is planned. Most medications can be continued unless told otherwise for sedation or contrast. If you’re anxious or claustrophobic, talk to the referrer or imaging team beforehand about open MRI, ear protection, music options or possible sedation. The checklist below covers the practical steps to help your appointment run smoothly.
- MRI preparation checklist:
Bring your referral and any implant or device documentation.
Remove all jewellery, watches, metallic makeup and removable dental appliances.
Wear comfortable, metal-free clothing or accept a gown if provided.
Follow fasting instructions only if contrast or sedation is scheduled; otherwise eat and drink as usual.
What Should You Wear and Avoid Before an MRI?
Wear loose, comfortable clothes without metal zips, snaps or underwires and avoid cosmetics with metallic particles that can create image artefacts. Remove credit cards, keys and electronic devices before entering the scan room. Hearing aids, removable dental work and non-permanent jewellery should be taken out and stored safely away from the scanner. If you’re unsure about clothing or accessories, call the imaging centre before your appointment to prevent unnecessary delays. Bringing prior imaging or implant information also helps the radiology team select the right coils and sequences.
How Can You Manage Claustrophobia During an MRI Scan?
Many people manage claustrophobia with non-pharmacological measures: tell the referrer and imaging team about your concerns, ask about open MRI if suitable, use music or earphones during the scan, and practise breathing and relaxation techniques. If these measures aren’t enough, mild sedation or anxiolytic medication can be arranged in advance with appropriate fasting and monitoring. Paediatric or special-needs patients may require anaesthesia services. Early communication lets the team plan accommodations and reduces motion artefact, helping preserve diagnostic quality.
What to Expect During and After an MRI Scan?
Your MRI appointment usually starts with arrival and safety screening, followed by changing into suitable attire if needed, positioning on the scanner table and placement of coils over the area of interest. Scan times vary by study — many scans take 20–60 minutes — and you’ll hear loud gradient noises that are reduced with ear protection and often background music. After the scan, images are processed and a radiologist reviews them; the report is sent to the referrer who will discuss the results and next steps with you. The timeline below gives a practical view of the typical patient experience.
- Typical MRI timeline for patients:
Arrival and safety screening (10–20 minutes).
Preparation and coil placement (5–15 minutes).
Scanning sequences (20–60 minutes depending on study).
Post-scan processing and radiologist reporting (variable; often 24–72 hours for routine outpatient reports).
How Long Does an MRI Scan Take and What Happens During It?
Individual MRI sequences last a few minutes each. A standard single-region scan usually totals 20–40 minutes, while multi-region or contrast-enhanced studies can extend to 45–90 minutes depending on protocol. During the scan you must lie still while the machine makes tapping or knocking noises; radiographers provide ear protection and often offer music and intercom communication. Emergency stop procedures are in place and a panic button may be given to the patient when appropriate, ensuring safety and immediate assistance if needed. After imaging, technologists check image quality and escalate any concerns to the radiologist before you leave.
How Are MRI Scan Results Interpreted and Communicated?
A radiologist with relevant subspecialty experience reviews and reports MRI studies, using clinical history and prior imaging to produce an interpretative report that is sent to the referrer; your referring clinician will usually discuss findings and next steps with you. Turnaround times depend on urgency and local workflow — urgent inpatient scans may be reported within hours, while routine outpatient reports commonly take 24–72 hours or longer for subspecialist reads. Ask your referrer how and when you’ll receive results, and request copies of reports if you need them for insurance or second opinions.
How Does MRI Compare to CT Scans?
MRI and CT are complementary tools. MRI gives superior soft-tissue contrast, detailed neurological views and multiplanar imaging without radiation. CT is faster, widely available and better for detecting acute haemorrhage, visualising bone detail and managing trauma. CT uses ionising X-rays and therefore carries radiation exposure, while MRI uses non-ionising radiofrequency energy and avoids that risk. The table below compares MRI, CT and ultrasound across key attributes to help decide which test is most appropriate for a given clinical question.
What Are the Key Differences Between MRI and CT Technology?
MRI uses magnetic fields and RF pulses to generate signals from hydrogen protons, giving excellent soft-tissue contrast and flexible sequences for tissue characterisation. CT measures X-ray attenuation to rapidly reconstruct cross-sectional images that excel at showing bone, acute haemorrhage and lung detail. MRI sequences can highlight fluid, fat or diffusion properties, while CT delivers consistent bone and air contrast with very fast acquisition — useful when patients can’t hold still. Safety procedures differ: MRI requires careful screening for ferromagnetic implants, while CT requires consideration of radiation dose and iodinated contrast allergies. Understanding the physics helps choose the safest, most diagnostic test for each clinical situation.
When Is a CT Scan More Suitable Than an MRI?
CT is favoured in acute trauma when speed and bone detail matter, in suspected intracranial haemorrhage where CT quickly detects blood, and in chest imaging where rapid, high-resolution air–tissue contrast is needed. CT is also used when MRI is contraindicated because of incompatible implants or when patient tolerance and time constraints make MRI impractical. MRI, by contrast, is preferred for complex neurological, musculoskeletal and soft-tissue problems where radiation avoidance and superior contrast improve diagnostic confidence. Clinicians balance diagnostic yield, urgency and patient factors when choosing the right modality.
What Diagnostic Imaging Services Does Life Medical Imaging Central Coast Offer?
Life Medical Imaging Central Coast is an independent, NATA‑accredited radiology clinic offering a full range of diagnostic imaging services to meet local needs. Our services include General CT, Cardiac CT, CT Angiography, Digital X‑ray and multiple ultrasound services (General, Vascular, Musculoskeletal, Obstetric and Gynaecological). We also provide interventional procedures — spinal and joint injections, biopsies and aspirations — as well as paediatric imaging, DEXA body composition and bone density scans, and platelet‑rich plasma (PRP) injections. This service mix complements the MRI information in this guide and supports continuity of care for patients on the Central Coast.
How Do Our Advanced CT and Ultrasound Services Complement MRI?
At Life Medical Imaging Central Coast, CT and ultrasound act as fast, effective alternatives or complements to MRI depending on the clinical question. CT is ideal for acute trauma and detailed bone assessment, while ultrasound is excellent for real‑time obstetric checks, vascular studies and image‑guided procedures such as joint injections and biopsies. When MRI is the preferred test but isn’t available locally, we can provide high‑quality CT or ultrasound assessments and help coordinate referrals to ensure patients access the most appropriate imaging. Discuss with your referrer whether a CT or ultrasound at our clinic will answer the clinical question or if an external MRI referral is required.
Where Can You Book CT and Ultrasound Scans on the Central Coast?
To book CT, ultrasound, X‑ray, interventional procedures, DEXA or PRP therapies at Life Medical Imaging Central Coast, contact the clinic using the practice’s listed channels and bring your referral and any prior imaging or implant documentation. Bookings normally require a clinician’s referral; our NATA accreditation reflects our commitment to diagnostic standards and quality assurance. If an MRI is specifically needed, we can advise on referral pathways or liaise with partners to help you access MRI services when indicated.
Frequently Asked Questions
What should I expect during the MRI scan process?
Your visit starts with safety screening and, if needed, changing into a gown. You’ll lie on a table that slides into the scanner while coils are placed over the area of interest. Most scans last 20–60 minutes and require you to remain still. The machine is noisy, but ear protection and music are usually provided to keep you comfortable. After the scan, images are processed and interpreted by a radiologist; results are communicated through your referrer.
How can I manage anxiety or claustrophobia before an MRI?
If you feel anxious or claustrophobic, tell your healthcare provider before the appointment. Options include booking an open MRI (when clinically suitable), using music or relaxation techniques, or arranging mild sedation. Discussing your concerns in advance helps the imaging team plan the most comfortable approach for you.
Are there any dietary restrictions before an MRI scan?
Dietary instructions depend on whether contrast or sedation is planned. If contrast is required, you may be asked to fast for a few hours beforehand. If no contrast or sedation is needed, you can usually eat and drink normally. Always follow the specific guidance given by your clinic.
What happens if I have a medical condition or implant?
Tell your referrer and the imaging team about any medical conditions or implants before the scan. Certain devices, such as non‑MR‑conditional pacemakers, may require specialist review and additional precautions. In some cases an alternative imaging test may be recommended to ensure safety and diagnostic quality.
How long does it take to receive MRI results?
Reporting times vary. Routine outpatient reports are often available within 24–72 hours; urgent cases can be reported within hours. Your referring clinician will discuss the findings with you — check with them for the expected timeline in your situation.
Can I bring someone with me to the MRI appointment?
You may bring a friend or family member for support, but they are usually not permitted inside the scan room because of the strong magnetic field. Check the facility’s visitor policy beforehand so you know what to expect.
What should I do if I feel uncomfortable during the scan?
If you become uncomfortable during the scan, communicate with the radiographer via the intercom. Many centres provide a panic button for immediate assistance. Let the imaging team know about any concerns before the scan so they can make proper arrangements and ensure your safety.
Conclusion
Knowing what to expect from MRI — its strengths, costs and safety considerations — helps you make informed choices about your care. Where MRI is the best option, it offers detailed diagnostic information without ionising radiation; where alternatives are preferable, CT and ultrasound provide complementary answers. For personalised advice or to arrange imaging on the Central Coast, contact Life Medical Imaging Central Coast — we’ll help you find the right test and guide you through the process.

