Pain Management Injections: Types, Benefits and How They Help Relieve Chronic Pain
Pain management injections are focused, minimally invasive procedures that deliver medication or biologic agents directly to the source of pain. They reduce inflammation, temporarily block pain signals, or encourage tissue repair — most commonly via corticosteroids (anti-inflammatory), local anaesthetics (nerve block) or platelet‑rich plasma (PRP, regenerative therapy). People with sciatica, osteoarthritis, herniated discs or chronic tendinopathy often choose injections to ease symptoms and improve function without immediate surgery. This article lays out the main injection types, how each works, typical outcomes and recovery timelines, the procedural steps and safety considerations, and how image guidance (CT, X‑ray/fluoroscopy and ultrasound) improves accuracy. We also explain local booking and referral options on the Central Coast. Read on to compare epidural steroid injections, facet joint injections, nerve root blocks, joint injections and PRP, learn how to prepare, what recovery looks like, and how to arrange appointments or referrals.
What Are the Main Types of Pain Management Injections?
Pain management injections cover several image‑guided procedures that deliver drugs or biologics to a specific anatomical pain source. Common options include epidural steroid injections, facet joint injections, nerve root blocks, intra‑articular joint injections and PRP. Each targets different tissues and pain mechanisms. Imaging (CT, X‑ray/fluoroscopy or ultrasound) is used routinely to confirm needle position, which improves safety and diagnostic value. The overview below summarises each procedure, its primary target and typical clinical indications so patients and referrers can compare choices clearly.
Different injection types at a glance:
- Epidural steroid injections: Steroid plus local anaesthetic delivered to the epidural space to reduce inflammation around nerve roots and relieve radicular pain.
- Facet joint injections: Steroid placed into a spinal facet joint (or around the medial branch nerve) to treat pain from facet arthropathy or spinal arthritis.
- Nerve root blocks: Local anaesthetic, often with steroid, injected near a spinal nerve root to diagnose and treat radicular pain.
- Intra-articular joint injections: Steroid or local anaesthetic injected into knee, hip, shoulder or sacroiliac joints for osteoarthritis or synovitis.
- PRP injections: Autologous platelet‑rich plasma used to stimulate healing in tendinopathy, some ligament injuries and early osteoarthritis.
These procedures differ by target and purpose — some are mainly diagnostic, others therapeutic. Knowing the differences helps set expectations and plan the next steps in care.
Intro to comparison table: The table below compares the main injection types by primary target, typical indication, imaging guidance and expected duration of relief so you can scan the differences quickly.
This comparison shows how clinicians select a procedure based on anatomy, likely pain cause and whether the goal is diagnostic or therapeutic. It prepares you for the following sections on mechanisms and outcomes.
How Do Epidural Steroid Injections Work for Back Pain?
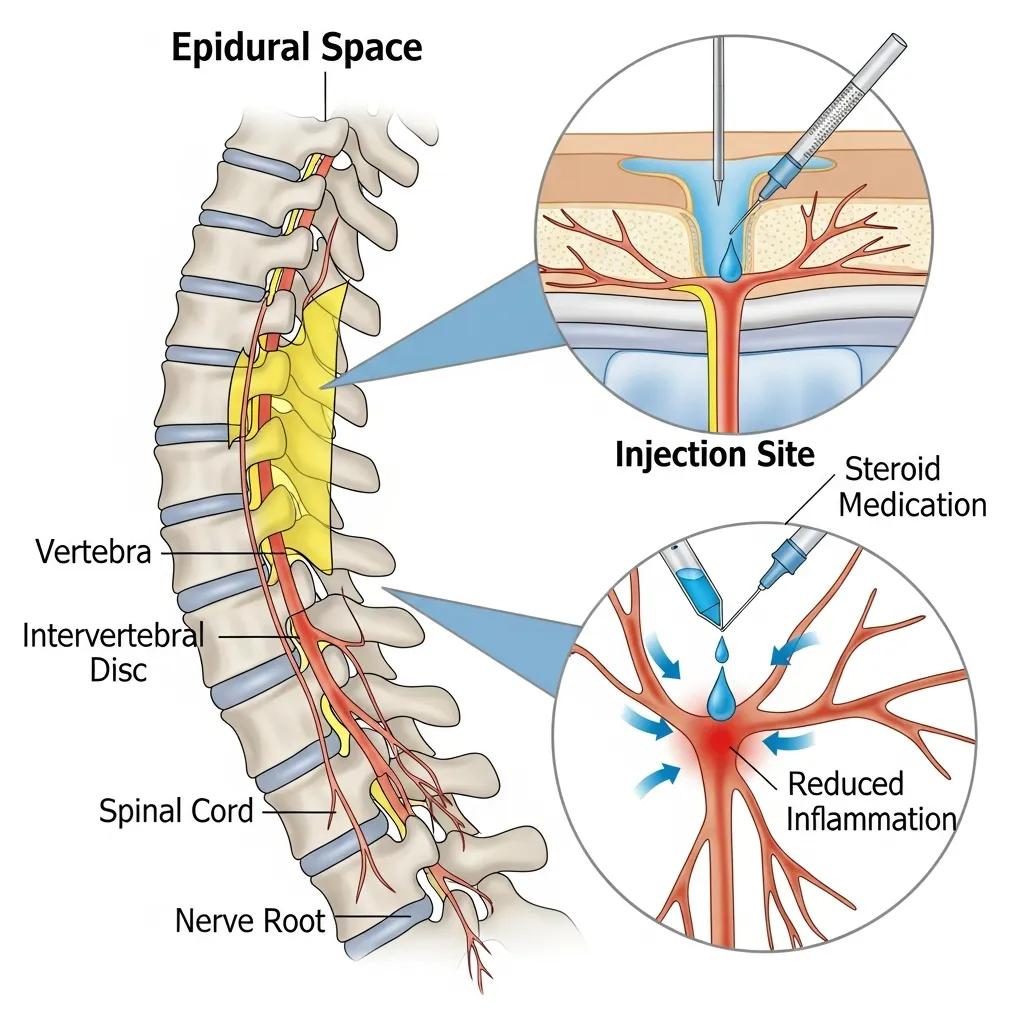
Epidural steroid injections place a corticosteroid and local anaesthetic into the epidural space that surrounds the spinal nerve roots. The steroid reduces inflammatory mediators and swelling around the nerve; the local anaesthetic provides rapid pain relief and helps confirm the pain source. Typical indications include sciatica from a herniated disc, degenerative spinal stenosis and radicular pain that follows a nerve‑root pattern. Patients may feel immediate benefit from the anaesthetic, with steroid effects developing over days; symptom relief can last from weeks to months for some people. Using fluoroscopy or CT to guide the needle improves accuracy and reduces complication risk, supporting both treatment effect and diagnostic clarity.
Epidural Corticosteroid Injections for Radicular Pain: A Systematic Review
This Cochrane‑style review examines epidural corticosteroid injections aimed at reducing local inflammation and relieving lumbosacral radicular pain. It updates earlier reviews and considers recent placebo‑controlled trials to clarify the evidence for symptom relief following epidural steroid delivery.
Epidural corticosteroid injections for radiculopathy and spinal stenosis: a systematic review and meta-analysis, J Friedly, 2015
What Are Facet Joint Injections and Their Role in Spinal Arthritis?
Facet joint injections deliver a small volume of steroid and local anaesthetic into the facet joint or around the medial branch nerves that supply it, aiming to reduce inflammation and interrupt pain signals. Facet joints are synovial joints that can become arthritic and cause axial back pain or referred discomfort to the buttock or posterior thorax. Diagnostic blocks help confirm facet‑mediated pain before moving to longer‑term treatments. Therapeutic injections can ease inflammation and allow rehabilitation with physiotherapy, while diagnostic medial branch blocks guide procedures such as radiofrequency ablation. Local anaesthetic effects are usually rapid; steroid benefits evolve over days. Repeat injections are considered based on symptom recurrence and clinical judgement, taking steroid frequency limits into account.
How Do Nerve Blocks and PRP Injections Provide Targeted Pain Relief?
Nerve blocks and PRP injections take different but complementary approaches. Nerve blocks interrupt pain transmission and provide diagnostic information; PRP aims to stimulate tissue repair and address underlying pathology. Selective nerve root and peripheral nerve blocks use local anaesthetic with or without steroid to temporarily abolish pain and identify the symptomatic nerve, guiding further care. PRP (platelet‑rich plasma) is an autologous concentrate that releases growth factors to support tendon and ligament healing or modulate joint tissues — useful for tendinopathy and early osteoarthritis. Imaging guidance (ultrasound for PRP; fluoroscopy or CT for many nerve blocks) ensures precise delivery and lowers the risk of injury to adjacent structures. The list below summarises common indications and helps match presentations to treatments.
Common indications for nerve blocks and PRP include:
- Sciatica and radicular pain: Nerve root blocks help confirm the source and can give temporary relief of nerve‑mediated leg pain.
- Tendinopathy (rotator cuff, Achilles, patellar): PRP is used to stimulate tendon healing and reduce chronic tendon pain.
- Ligament injuries and early joint degeneration: PRP may improve tissue quality and symptoms where biological repair is appropriate.
Effectiveness of Epidural Steroid Injections for Lumbar Nerve Root Compression
This randomised, controlled trial compared epidural steroid injections with intramuscular injections to evaluate symptom relief for lumbar nerve‑root compression. Ninety‑three patients were followed with validated outcome measures, providing insight into clinical effectiveness for those being considered for surgery.
Epidural steroid injection for nerve root compression: a randomised, controlled trial, D Griffin, 2005
In short: nerve blocks offer fast diagnostic and sometimes therapeutic benefit by interrupting nociceptive signals, while PRP has a slower onset aimed at regeneration and longer‑term symptom control. Often clinicians use blocks to localise pain and then consider regenerative therapy where appropriate to optimise outcomes.
What Conditions Can Nerve Root Blocks Treat?
Nerve root blocks are used when pain radiates along a specific spinal nerve. They are effective for sciatica from lumbar disc herniation, radicular pain from spinal stenosis and selected cases of cervical radiculopathy. The injection — usually local anaesthetic with or without steroid — is placed near the affected nerve root to reduce inflammation and confirm the nerve as the pain source. A predictable, reproducible decrease in pain shortly after the block helps distinguish nerve‑root pain from referred or myofascial pain. Typical presentations include sharp, shooting arm or leg pain following a dermatomal pattern, sometimes with sensory changes or altered reflexes. Follow‑up commonly includes physiotherapy, activity modification and consideration of further interventions based on symptoms and functional goals.
How Does Platelet-Rich Plasma Therapy Help Joint and Soft Tissue Pain?

PRP is made from a patient’s own blood by concentrating platelets and injecting that concentrate into injured tendons, ligaments or joints to harness growth factors that support tissue repair. Platelets release bioactive proteins — for example platelet‑derived growth factor and transforming growth factor‑beta — that recruit reparative cells and modulate inflammation. This can lead to reduced pain and improved function over weeks to months. Common uses include chronic tendinopathies (such as tennis elbow or Achilles tendinopathy), early osteoarthritis and partial ligament injuries where biological healing is desirable. PRP injections are performed under ultrasound guidance for accurate placement, usually require a short recovery period and may be given as a single treatment or a short course depending on the condition and response.
What Are the Benefits and Outcomes of Pain Management Injections?
Pain management injections can provide meaningful benefits: pain reduction, less inflammation, improved mobility and diagnostic clarity to guide ongoing care. Corticosteroids reduce inflammatory mediators around nerve roots and joint synovium, often producing measurable pain score improvements and greater activity tolerance. Local anaesthetics give immediate relief that can confirm the treated structure and enable early rehabilitation. PRP aims for longer‑term tissue modulation by promoting collagen synthesis and matrix remodelling, with patient‑reported improvements typically appearing over weeks. Below is a concise breakdown of common agents, their mechanisms and expected clinical outcomes to help set realistic expectations.
Intro to mechanism table: The following table links common injected agents to their mechanism of action and typical clinical outcomes seen in practice.
Key benefits patients may expect include:
- Pain reduction: Targeted treatments lower nociceptive and inflammatory signals.
- Improved mobility: Less pain often allows more effective physiotherapy and functional gains.
- Diagnostic clarity: A response to local anaesthetic helps identify the pain source.
- Potential regenerative effect: PRP can support tissue healing in selected cases.
Epidural Corticosteroid Injections for Sciatica: A Cochrane Review Update
This updated review examines the use of epidural corticosteroid injections for lumbosacral radicular pain (sciatica). It summarises recent placebo‑controlled trials and previous evidence to help clinicians weigh benefits and limitations when considering epidural steroid treatment.
Epidural corticosteroid injections for lumbosacral radicular pain, CB Oliveira, 1996
Outcomes depend on diagnosis, technique and choice of imaging guidance. Combining injections with tailored rehabilitation typically gives the best long‑term results. On the Central Coast, Life Medical Imaging Central Coast provides imaging‑guided interventional procedures including spinal and joint injections, biopsies and aspirations, and PRP therapy. If you or your referrer would like to discuss suitability, the clinic can advise on imaging needs, procedural planning and how injections might fit your overall treatment pathway.
How Do Injections Reduce Inflammation and Improve Mobility?
Corticosteroids reduce production of inflammatory mediators and lower vascular permeability at the targeted site, which decreases nerve irritation and joint swelling. That biological effect often translates to lower pain scores and better range of motion. Local anaesthetics block nerve conduction temporarily, allowing patients to participate in rehabilitation without immediate pain limiting movement. Short‑term benefits can restore sleep and daily activity tolerance; over the medium term, reduced pain enables physiotherapy and progressive loading to rebuild strength and function. When injections are combined with a rehabilitation plan they act as a bridge to longer‑term recovery rather than a standalone cure.
Can Pain Injections Serve as Diagnostic Tools?
Yes — diagnostic injections use local anaesthetic to temporarily numb a suspected pain generator. If pain resolves reliably after the block, clinicians gain confidence that the targeted structure is responsible and can plan further treatment accordingly. Examples include medial branch blocks for facet pain and selective nerve root blocks for radicular pain. Diagnostic blocks are particularly helpful when imaging is unclear or when multiple potential pain sources exist, because they provide functional confirmation beyond anatomy. Results must be interpreted alongside clinical history and examination, and clinicians remain aware of false positives and the transient nature of the effect.
What Should Patients Expect During and After Pain Management Injection Procedures?
Expect a clear, stepwise process: pre‑procedure assessment and consent, image‑guided needle placement during the procedure, then a short recovery period with aftercare instructions. Preparation includes reviewing medications (especially anticoagulants), arranging transport home and understanding risks and benefits — these steps lower complication risk and improve procedural efficiency. During the procedure, CT, fluoroscopy or ultrasound confirms needle placement while sterile technique and local anaesthesia minimise discomfort; many procedures are day‑case and light sedation is available if needed. Aftercare typically involves activity modification, watching for minor reactions such as soreness, and follow‑up to assess response and plan rehabilitation. Immediate change from local anaesthetic helps clinicians interpret success and next steps.
Preparation checklist intro: Before your injection, follow this short checklist to help ensure safety and the best possible outcome.
- Medication review: Tell clinicians about anticoagulants and other medicines that may need temporary adjustment.
- Transport arranged: Organise a responsible adult to drive you home if sedation or anaesthesia is used.
- Fasting and paperwork: Follow any fasting instructions and bring referral letters or prior imaging as requested.
Summary paragraph and clinic process note: Proper preparation minimises risks and helps a smoother recovery. Life Medical Imaging Central Coast uses image guidance (CT, X‑ray/fluoroscopy, ultrasound) for needle placement and provides clear pre‑ and post‑procedure instructions. The clinic can also help with appointment bookings and referral queries.
How Should You Prepare for Your Pain Management Injection?
Preparation starts with a clinical assessment and review of recent imaging and medications to confirm suitability and identify contraindications (for example, active infection). Discuss anticoagulant therapy with your referrer and the clinic, as some blood thinners require temporary modification to reduce bleeding risk. Practical steps include arranging transport, wearing loose clothing for access to the injection site and bringing referral notes or imaging when requested. Confirm fasting or sedation instructions with the clinic beforehand so the team can tailor preparation for CT, fluoroscopy or ultrasound guidance.
What Is the Recovery Process and Aftercare Following Injections?
Immediate recovery usually involves a short observation period during which staff check vital signs and scan for early reactions. The local anaesthetic effect is often felt within minutes and steroid‑related improvement may follow over several days. Minor effects include temporary soreness at the injection site, facial flushing or a short steroid flare (a brief increase in pain) that typically settles with conservative care. Patients are encouraged to resume activities gradually, start physiotherapy if recommended, and report red flags such as fever, worsening neurological symptoms or uncontrolled pain. Follow‑up with your referrer or the imaging clinic will assess response, consider repeat injections where appropriate and coordinate ongoing rehabilitation.
What Are the Risks and Side Effects of Pain Management Injections?
When performed under image guidance by experienced practitioners, pain management injections have a favourable safety profile, but like all procedures they carry both common, transient effects and rare, serious complications. Typical short‑term effects include local soreness, transient steroid‑related symptoms (hot flushes, fluid retention) and brief pain flares — usually self‑limiting and manageable. Rare but important risks include infection, bleeding, allergic reaction or neurological injury; these are uncommon when sterile technique and imaging guidance are used. The table below summarises procedure‑specific risks so patients can discuss benefits and risks with their clinician.
Intro to risk table: The following table categorises procedure‑specific risks and provides context on frequency and clinical implications.
Summary paragraph: Knowing the risk profile supports informed consent and helps clinicians tailor care, balancing expected benefit against potential adverse events. Patients with bleeding disorders, uncontrolled infection or certain systemic conditions may not be suitable candidates; discuss alternatives with your referrer.
Are Pain Management Injections Safe for Chronic Pain?
For many people with chronic pain, injections are a safe and useful part of a multimodal management plan when chosen appropriately and performed by experienced clinicians. Safety depends on correct patient selection, good technique and moderation of cumulative steroid exposure. Evidence supports using injections both diagnostically and therapeutically, while regenerative options like PRP may be offered when suitable. Long‑term management usually combines injections with physiotherapy, medications and lifestyle measures rather than relying solely on procedures. Discuss your long‑term goals with your referrer so injections are integrated into a plan that prioritises function and quality of life.
What Side Effects Should Patients Be Aware Of?
Expect minor, short‑lived effects such as local soreness, temporary numbness from local anaesthetic and brief steroid‑related flares; these typically settle with simple analgesics and rest. Less common effects include signs of infection (fever, increasing redness), bleeding at the site and systemic steroid effects such as raised blood glucose in susceptible people. Neurological warnings — new weakness, severe or progressive numbness, difficulty with bladder or bowel control — require immediate medical attention. The clinic will give clear instructions on when to seek help so any complications are identified and treated promptly.
How Can You Book Pain Management Injection Consultations on the Central Coast?
Arranging a pain management injection consultation on the Central Coast is straightforward for patients and referrers: submit a clinical referral, provide relevant imaging for review, and schedule an appointment with the interventional radiology team or pain clinic. Referrers should include a clinical history and copies of MRI, CT or X‑ray when available so the clinic can triage urgency and plan the procedure. If you don’t yet have a specialist referral, speak to your GP about referral options so the imaging team can assess suitability and advise the pre‑procedure pathway. The steps below outline a typical booking process.
Steps to arrange an injection consultation:
- Obtain a clinical referral: Ask your GP or specialist to provide a referral with clinical history and any recent imaging.
- Contact the imaging clinic: Call the clinic to check appointment availability and pre‑procedure guidance.
- Provide documents: Send or bring referral letters and copies of recent imaging so the team can review before booking.
Summary paragraph and contact details: These steps streamline booking and let the imaging team prepare for safe, image‑guided procedures. Life Medical Imaging Central Coast is an accredited, independent radiology clinic offering advanced diagnostic imaging and interventional procedures — spinal and joint injections, biopsies and aspirations, and PRP therapy. For appointment enquiries please call 02 4326 7000. The clinic can provide information about services and help facilitate bookings or referrals.
Which Life Medical Imaging Locations Offer Pain Management Injections?
Life Medical Imaging Central Coast operates multiple clinic sites across the Central Coast with accredited imaging and interventional capabilities; availability of specific procedures varies by location and changes over time. Contact the imaging team by phone to confirm which sites currently perform spinal injections, joint procedures or PRP therapy. The clinic highlights NATA accreditation, modern imaging equipment and experienced staff to support safe, precise interventions and patient comfort. Calling the service gives the most up‑to‑date information on locations, scheduling and pre‑procedure requirements.
How Do Referring Doctors and Patients Arrange Appointments?
Referrers typically submit a referral letter and required imaging; the imaging service reviews the referral, triages urgency and contacts the patient to arrange an appointment and pre‑procedure assessment. Patients should ensure their referrer includes a clear clinical history, current medications and copies of recent imaging to speed assessment and avoid repeated tests. For direct enquiries, the clinic phone line will explain referral requirements, booking steps and preparation instructions; urgent cases are prioritised by clinical need. Timelines depend on local demand and clinical urgency, and the imaging team will advise on estimated wait times and any interim pain‑management measures.
- Referrer submits clinical referral and imaging: Ensures appropriate triage and planning.
- Clinic contacts patient: Arranges appointment and pre‑procedure instructions.
- Pre‑procedure review and scheduling: Confirms medication adjustments and logistics.
This stepwise process helps coordinate referrers, imaging services and patients to deliver safe, image‑guided pain management procedures on the Central Coast.
Frequently Asked Questions
What is the typical recovery time after a pain management injection?
Recovery varies by injection type and individual response. Local anaesthetic often gives immediate, short‑lived relief; corticosteroid or PRP benefits can take days to several weeks to appear. Most people can resume normal activities within a day or two, though strenuous activity may be limited briefly. Follow the aftercare instructions from your healthcare team to optimise recovery.
Are there any long-term effects associated with pain management injections?
Long‑term effects depend on the injection type and frequency. Repeated corticosteroid injections can have potential adverse effects — for example on joint cartilage or systemic steroid exposure — so clinicians usually limit their frequency. PRP is regenerative and generally has fewer long‑term risks, but responses vary. Regular follow‑up helps monitor outcomes and adjust treatment plans as needed.
How do I know if pain management injections are right for me?
Determining suitability requires a clinical assessment by a healthcare professional. Factors considered include pain type and severity, prior treatments, imaging findings and overall health. A careful review, including relevant imaging and a discussion of goals, will help identify whether injections are an appropriate option. Talk to your clinician about your expectations and concerns to make a shared decision.
Can pain management injections be repeated, and how often?
Injections can be repeated, but frequency depends on the procedure and individual factors. Corticosteroid injections are usually limited in number (often to a few per year for the same site) to reduce systemic effects. PRP may be repeated based on clinical response and the condition treated. Ongoing review ensures repeat treatments are appropriate and safe.
What should I do if I experience side effects after an injection?
Contact your healthcare provider promptly if you experience side effects. Common issues such as temporary soreness, increased pain or mild swelling usually resolve on their own. Seek immediate attention for severe symptoms — for example fever, marked swelling, worsening neurological signs or severe uncontrolled pain. Your clinician will advise on managing side effects and whether further assessment is needed.
Are pain management injections covered by health insurance?
Insurance coverage varies by provider and plan. Many insurers cover medically necessary injections, but pre‑authorisation or specific documentation may be required. Check with your insurer for details on coverage, out‑of‑pocket costs and any referral or pre‑approval steps. The clinic can also discuss likely costs and payment options when you enquire.
Conclusion
Pain management injections provide targeted options to reduce inflammation, ease pain and improve function for many chronic conditions. Understanding the types of injections, how they work and what to expect helps you make informed choices about your care. If you are considering these treatments, contact our clinic for personalised advice and to discuss the best pathway for your situation. Reach out today to take the next step toward better function and less pain.

