PRP Injections — a clear guide to platelet‑rich plasma, how it works and what to expect
Platelet‑rich plasma (PRP) uses a concentrated portion of your own blood to encourage healing and relieve pain in injured or degenerative tissues. This guide explains what PRP is, how platelet growth factors support tissue repair, and when PRP may be a non‑surgical option for musculoskeletal pain. Many people want clear, evidence‑based answers about PRP’s effectiveness, realistic timelines and the procedure itself — this article provides practical, clinical information. You’ll learn the biological basis of PRP, which conditions tend to respond best, why image‑guided injections matter, and what to expect during recovery. Practical sections cover the patient journey at an imaging clinic, benefits and risks, preparation and follow‑up, and how to ask about PRP locally. Throughout we reference current research and clinical reasoning to help patients and referring clinicians make informed choices about PRP injections.
What is platelet‑rich plasma therapy and how does it work?
PRP is an autologous blood concentrate: we draw a small sample of your blood, centrifuge it to separate components, then use the platelet‑rich fraction to deliver growth factors to a targeted area. Platelets release signalling molecules that help modulate inflammation, attract reparative cells and stimulate cell proliferation. Because the product comes from the patient’s own blood, the risk of allergic reaction is very low. Clinical studies show many people notice symptom improvement within weeks, with tissue remodelling and functional gains most commonly seen over 6–12 weeks. These biological effects explain why PRP is often placed precisely into tendons, ligaments or joint spaces using image guidance.
Novel applications of platelet concentrates in tissue regeneration
ABSTRACT: Recent reviews summarise how platelet concentrates — including PRP, platelet‑rich fibrin and related products — are prepared from centrifuged blood and used in soft and hard tissue engineering. Key components such as growth factors, fibrin matrix and platelets play central roles in wound healing. Current research is exploring ways to enhance these autologous products, for example through improved preparation protocols or preservation techniques, to better meet clinical needs in tissue restoration. The review highlights recent advances and practical considerations for using platelet concentrates in regenerative medicine.
Life Medical Imaging Central Coast provides image‑guided PRP as part of our interventional services for patients seeking precise, imaging‑assisted injections. This note helps patients know an accredited imaging clinic offers PRP; the sections that follow focus on clinical education about how PRP works and when it may be appropriate.
What are the key components of PRP and what do they do?
PRP’s effect comes from platelets suspended in plasma, which deliver growth factors such as PDGF, VEGF and TGF‑beta that coordinate repair. Platelet granules release signals that recruit reparative cells; plasma supplies a protein‑rich scaffold; together they create a local environment that supports healing. PDGF encourages cell proliferation and migration, VEGF promotes new blood vessel formation, and TGF‑beta helps regulate extracellular matrix production and remodelling. Using the patient’s own blood limits immunologic risk while concentrating biological signals at the site that needs repair — which is why autologous PRP is commonly used in orthobiologic practice.
This component‑level overview leads into how those signals translate into tissue repair and symptom improvement.
How does PRP promote tissue repair and reduce pain?
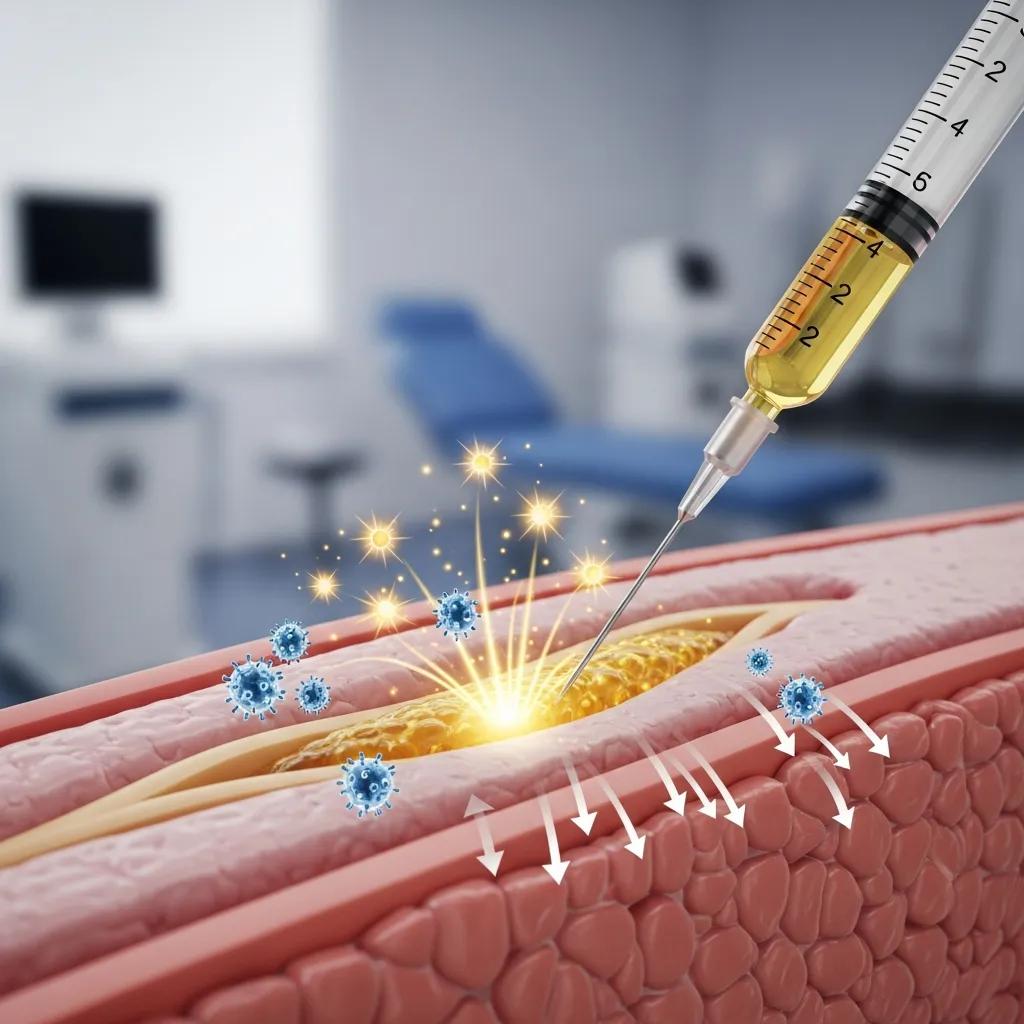
Once injected, platelets release growth factors that trigger a cascade of events: modulation of inflammation, recruitment of reparative cells, new blood vessel formation, collagen synthesis and matrix remodelling. An early, short‑lived inflammatory phase can cause increased discomfort for 24–72 hours before pain starts to settle as healing progresses. Meaningful pain relief and improved function typically emerge over 6–12 weeks, reflecting the time needed for collagen realignment and improved tissue quality. For this reason many PRP protocols include a period of graded rehabilitation and clinical review to support the biological effects while restoring strength and mechanics.
With that timeline in mind, the next section explains which musculoskeletal problems most commonly respond to PRP.
Which conditions can PRP injections treat effectively?
PRP is used for a range of musculoskeletal problems where a biological stimulus can support repair — particularly degenerative joints and chronic tendinopathies. The strongest evidence exists for some indications, such as early to moderate knee osteoarthritis and certain tendinopathies; results are more variable for other conditions and depend on factors like lesion chronicity and patient characteristics. Deciding on PRP versus other treatments should consider the condition, severity, previous therapies and patient goals. Below is a quick, scannable list of common indications and what to expect.
Common indications for PRP injections include:
- Knee osteoarthritis: to reduce pain and improve function, especially in early‑to‑mid stage disease.
- Tendinopathies (for example, lateral epicondylitis or Achilles tendinopathy): to stimulate tendon repair when conservative care hasn’t helped.
- Ligament and muscle injuries: to support recovery and reduce symptoms in selected cases.
- Plantar fasciitis: for chronic plantar fascia pain that hasn’t responded to standard measures.
These summaries lead into more detailed evidence and protocol notes for joints and tendon injuries below.
How is PRP used for joint pain and osteoarthritis?
For joint pain, particularly knee OA, PRP is injected into the joint (intra‑articularly) to deliver growth factors that may reduce inflammation and support the joint environment and cartilage metabolism. Protocols range from a single injection to a short series spaced a few weeks apart, with follow‑up to assess symptom response and function. Recent trials show modest to moderate pain relief and improved patient‑reported outcomes in early‑to‑moderate knee OA, but results vary by PRP formulation and patient factors. Careful patient selection — for example, avoiding end‑stage disease — and combining PRP with physiotherapy to optimise joint mechanics can improve results.
Next we cover tendon and soft‑tissue uses, where image guidance is commonly used to increase precision.
Can PRP help with tendon, ligament and muscle injuries?
PRP is commonly used for chronic tendinopathies, partial‑thickness tendon tears and selected ligament or muscle injuries when conservative care hasn’t worked. Ultrasound guidance enables precise placement into degenerated tendon zones or at tendon insertions, improving the chance of a therapeutic effect. Clinical responses vary: many people report meaningful pain relief and return of function over 6–12 weeks, but outcomes depend on how chronic the lesion is, adherence to rehabilitation and PRP concentration. We usually recommend combining PRP with structured physiotherapy that emphasises progressive loading so biological repair converts into lasting functional gains.
Explaining the procedure and image‑guided delivery at an imaging clinic helps clarify the patient journey that follows.
What is the PRP injection procedure at Life Medical Imaging Central Coast?
In an imaging clinic the PRP procedure combines diagnostic assessment, sterile blood processing and image‑guided injection to maximise precision and safety. The typical patient pathway includes referral review, targeted imaging (for example musculoskeletal ultrasound), a consultation and consent, blood draw and centrifugation, then ultrasound‑guided injection into the identified target and brief post‑procedure observation. Image guidance helps ensure PRP is delivered into the tendon, ligament or joint space as intended, reducing off‑target delivery and improving the chance of benefit. Our interventional service is designed to support this coordinated workflow and to communicate results and follow‑up plans with referring clinicians.
- Referral and pre‑procedure review: we check clinical details and any prior imaging to confirm suitability.
- Clinic consultation and consent: a radiologist or interventional clinician discusses the procedure, risks and expected outcomes.
- Blood draw and PRP preparation: a venous sample is processed in a centrifuge to concentrate platelets.
- Image‑guided injection: ultrasound is used to target the tendon, ligament or joint for precise PRP placement.
- Immediate observation and aftercare advice: a short monitoring period followed by clear instructions on activity and follow‑up.
This step‑by‑step summary sets expectations and is followed by a table that describes each stage with typical times and patient actions.
What steps are involved from consultation to injection?
On the day of treatment you’ll have a pre‑procedure briefing and consent confirmation, and any baseline imaging if needed. A venous blood draw is taken and PRP prepared in a sterile area; centrifugation typically takes 10–20 minutes while the clinician confirms anatomy with ultrasound. During the image‑guided injection the clinician places the needle under real‑time ultrasound into the affected tendon, ligament or joint and administers the PRP concentrate. After the procedure you’ll be observed briefly for immediate reactions and given personalised advice on activity, pain relief options and follow‑up to monitor progress.
How does image‑guided PRP improve precision and safety?
Image guidance — most commonly musculoskeletal ultrasound — lets the clinician visualise the needle tip and target tissue in real time, reducing the risk of injecting non‑target structures and increasing the chance platelets reach the pathological zone. Ultrasound also allows assessment of tendon integrity, bursal spaces and joint effusions so injections can be aimed at the area most likely to benefit. This precision lowers collateral tissue trauma and supports better outcome tracking because the treated lesion is documented before and after the procedure. An imaging clinic setting reinforces sterile technique and procedural oversight, which enhances safety and patient confidence in the intervention.
With the procedure and guidance covered, the next sections summarise benefits and risks so expectations are realistic.
What are the benefits and potential risks of PRP therapy?

PRP is an autologous, biologically based treatment that can reduce pain and support tissue healing with a lower allergy risk than donor‑derived injectables. Reported benefits include pain reduction, improved function and the potential to delay or avoid surgery for selected patients when combined with rehabilitation. Common risks are usually minor — local soreness, bruising or a transient inflammatory flare — and serious complications such as infection are uncommon when sterile technique and image guidance are used. Open discussion of benefits and risks helps set realistic expectations and supports shared decision‑making between patients and their referring clinicians.
Benefits of PRP therapy include:
- Reduced pain through inflammation modulation and stimulation of tissue repair.
- Improved function and return to activity when combined with appropriate rehabilitation.
- An autologous approach that lowers the risk of allergic reactions compared with donor products.
While many patients experience meaningful improvement, the degree and timing of benefit vary by condition and individual factors. Realistic expectations and coordinated follow‑up are important.
Risks and common side effects include:
- Local soreness, swelling or bruising at the injection site.
- A temporary increase in pain (a post‑injection flare) for 1–3 days.
- Rare complications such as infection or injury to nearby structures if sterile technique or targeting are inadequate.
Most adverse effects are minor and resolve on their own; careful sterile practice, image‑guided placement and appropriate patient selection substantially reduce risks.
What are the main advantages of PRP injections for pain and healing?
PRP delivers concentrated, autologous growth factors directly to damaged tissue, which can help modulate inflammation, encourage collagen production and support new vessel growth in areas that struggle to heal. For people seeking alternatives to repeated corticosteroid injections or early surgery, PRP is a regenerative option that focuses on biological repair rather than only symptom suppression. Its autologous nature lowers immunologic risk, and combining PRP with rehabilitative loading protocols helps translate biological repair into lasting functional improvement. Benefits are often measurable within 6–12 weeks, and adherence to rehabilitation commonly influences long‑term outcomes.
What side effects or risks should patients be aware of?
Expect possible short‑term local soreness, bruising and a transient pain flare after a PRP injection; these reactions usually settle in a few days and can be managed with rest and simple analgesics as advised. Infection is rare but is a recognised procedural risk, so sterile technique and monitoring for red‑flag symptoms such as increasing pain, spreading redness or fever are important. Active infection at the injection site or systemic infection are contraindications to PRP. Patients on anticoagulant therapy or with bleeding disorders need specialist assessment before proceeding. Any unexpected or severe symptoms after injection should prompt urgent review by the treating clinician or referring doctor.
How should patients prepare for PRP therapy and what is recovery like?
Preparation for PRP is straightforward but important for safety and best results. Discuss current medications, recent infections and any bleeding history with the treating clinician beforehand. Common advice includes avoiding non‑prescribed NSAIDs for a short period before the injection if recommended, since these drugs can blunt platelet activity, and arriving well hydrated for the blood draw. Plan transport and allow for activity limitations on the day if local anaesthetic or sedation is used, and bring any recent imaging or referral notes to the appointment. Clear preparation helps the clinic process your PRP efficiently and supports sterile, image‑guided targeting.
Practical pre‑procedure checklist and next steps are outlined below for clarity.
- Bring your referral and any recent relevant imaging or reports.
- Tell the clinician about all medications, allergies and recent infections.
- Follow medication advice from your referring doctor or the clinic — especially regarding anticoagulants and NSAIDs.
- Arrange transport and allow time for the appointment, which includes blood processing and observation.
These preparation steps lead into what to expect during recovery and the typical follow‑up schedule described next.
What pre‑procedure guidelines should patients follow?
Before PRP, make sure your medical history and current medications are communicated clearly so any contraindications — such as active infection or uncontrolled bleeding risk — are identified. Many clinicians recommend pausing non‑prescribed NSAIDs in the days before the injection to avoid reducing platelet function, while continuing essential prescribed medicines unless advised otherwise by the prescriber. Fasting is usually not required, but being comfortable and well hydrated helps the blood draw and centrifugation process. Planning for a short rest period after the procedure and arranging transport if needed improves safety and reduces day‑of stress.
These guidelines lead into a practical week‑by‑week view of recovery and expected milestones.
What can patients expect during recovery and follow‑up?
In the first 24–72 hours after injection you may have local discomfort or a pain flare that typically eases with conservative measures and rest. Structured rehabilitation usually starts a few days to a week after the injection, depending on the treated tissue. Progressive improvement in symptoms and function is commonly reported over 4–12 weeks, with clinical or imaging reassessment scheduled to monitor response and plan next steps if needed. Some patients benefit from a single injection, others from a short course spaced weeks apart; follow‑up helps decide whether additional treatments or alternative approaches are required. Clear communication between you, your referring clinician and the imaging team ensures the best sequencing of rehabilitation and any further interventions.
Why choose Life Medical Imaging Central Coast for PRP injections?
Life Medical Imaging Central Coast delivers PRP within an accredited imaging and interventional service model that prioritises precise, image‑guided delivery and integrated diagnostic expertise. Our accredited facility and experience in musculoskeletal imaging support accurate diagnosis, targeted treatment planning and real‑time guidance during PRP injections. This imaging‑first approach can improve procedural accuracy and safety compared with blind injections, and helps referring clinicians and patients understand the anatomical reasons behind treatment decisions. For patients who value diagnostic clarity and procedural precision, an imaging clinic provides a streamlined pathway from assessment to intervention and follow‑up.
- Accredited imaging services that support accurate diagnosis and interventional care.
- Image‑guided PRP injections to improve targeting and reduce procedural risk.
- An integrated pathway for assessment, treatment and follow‑up within an imaging clinic environment.
This information leads directly to practical booking guidance and how to make enquiries or send referrals.
How does Life Medical Imaging’s expertise enhance PRP outcomes?
Providing PRP from an imaging clinic improves outcomes mainly through precise anatomic targeting with ultrasound and interventional oversight that documents lesion location and treatment placement. Imaging expertise lets clinicians tailor the injection approach to the specific pathology — intra‑articular, intratendinous or at ligament insertions — reducing off‑target delivery and increasing the chance of a therapeutic effect. Working within an interventional imaging service also enables clear communication back to referring clinicians about findings and recommended rehabilitation steps, supporting multidisciplinary care and outcome tracking. These capabilities make an imaging clinic a sensible choice for PRP when precision and diagnostic clarity matter.
This explanation naturally moves to how patients and referring doctors can start the booking process or request further information.
How can patients book appointments or get more information?
If you or your referring clinician would like to discuss PRP options or arrange an appointment, contact Life Medical Imaging Central Coast via the clinic website or our Google Business Profile. Referrers should include relevant clinical notes and any recent imaging so we can triage suitability for PRP and plan any diagnostic imaging needed beforehand. Our interventional team can advise on preparation, expected timelines and follow‑up after reviewing the referral and clinical information. For patients, this referral‑and‑review step helps create a safe, efficient pathway from initial assessment to image‑guided PRP injection when appropriate.
This final administrative guidance closes the patient journey while emphasising coordinated care and clear referral communication.
Frequently Asked Questions
What is the typical recovery timeline after a PRP injection?
Recovery varies by individual and condition, but commonly you may have local discomfort or a pain flare in the first 24–72 hours. Most people see progressive improvement in symptoms and function over 4–12 weeks. Rehabilitation usually starts a few days to a week after the injection, and follow‑up reviews help determine whether further treatment is needed.
Are there any specific contraindications for PRP therapy?
Yes. Active infection at the injection site, uncontrolled bleeding disorders and some anticoagulant therapies can make PRP unsuitable. Certain systemic conditions or recent surgery in the target area should be discussed with your clinician to ensure safety and effectiveness. Your treating team will review your history to confirm suitability.
How does PRP compare to other treatment options for musculoskeletal pain?
PRP aims to promote biological repair rather than only relieve symptoms. Corticosteroid injections can offer rapid pain relief but may have negative long‑term effects on tissues. PRP is autologous, reducing allergy risk, and focuses on encouraging healing — making it an option for patients wanting to avoid repeated steroids or surgery. Outcomes vary, so choice of treatment should be individualised.
What should patients expect during the PRP injection procedure?
The procedure includes a consultation, blood draw and image‑guided injection. After reviewing your history and any imaging, we take a blood sample and process it to concentrate platelets. The clinician then uses ultrasound to guide the injection to the target area. You’ll be monitored briefly afterwards and given clear aftercare instructions.
Can PRP therapy be combined with other treatments?
Yes. PRP is often combined with rehabilitation — for example physiotherapy that provides progressive loading — to enhance recovery. This combined approach helps convert biological repair into lasting functional improvements. Discuss a coordinated treatment plan with your healthcare team to optimise results.
How can patients ensure the best outcomes from PRP therapy?
To get the best results, follow pre‑procedure guidance (for example advice about NSAIDs and hydration), engage in the recommended rehabilitation programme and attend scheduled follow‑ups. Clear communication with your clinician about medications, symptoms and progress helps tailor care and improve outcomes.
Conclusion
PRP therapy offers a natural, autologous option to support healing and reduce pain in selected musculoskeletal conditions. By using the body’s own growth factors and delivering them precisely with image guidance, many patients achieve meaningful improvements in function and pain — often avoiding more invasive treatments. Understanding how PRP works, who may benefit and what to expect helps you make an informed decision about your care. For more information about PRP and whether it might suit you, contact Life Medical Imaging Central Coast.

