What You Need to Know About CT Scans: Uses, Procedure, and Safety
A computed tomography (CT) scan uses rotating X‑rays and detector arrays to build detailed cross‑section images of the body. This guide explains how CT works, the most common clinical uses, what to expect before and during your appointment, and how results are reported — written for both patients and referring clinicians. We address common concerns about radiation and contrast, and provide clear preparation checklists, timelines and practical tips. You’ll also find a plain‑language overview, concise technical notes for referrers, a comparison with MRI and ultrasound, a transparent radiation dose table and quick‑reference lists to help with decision making. The emphasis is on clear, actionable information: when CT is the best choice, ways to limit dose, typical scan pathways and how images affect clinical care.
What Is a CT Scan and How Does It Work?
A CT (computed tomography) scan collects multiple X‑ray images from different angles and uses reconstruction software to create cross‑sectional views of anatomy quickly and accurately.
The scanner combines a rotating X‑ray tube, detector arrays that measure transmitted radiation, and reconstruction algorithms to produce high‑resolution slices. This method improves diagnostic accuracy for fractures, haemorrhage and complex anatomy.
CT’s main advantages are speed and spatial resolution: it images bone, air‑filled lungs and acute bleeding more reliably than many other tests, which is why it is so valuable in emergency settings.
The table below summarises core CT components and their roles for referrers and patients who want a concise technical breakdown.
Knowing these parts explains why CT is preferred for fast, high‑resolution imaging in trauma and vascular studies, and helps referrers select appropriate protocols and patients understand why preparation or contrast may be needed.
What Are the Different Types of CT Scans?
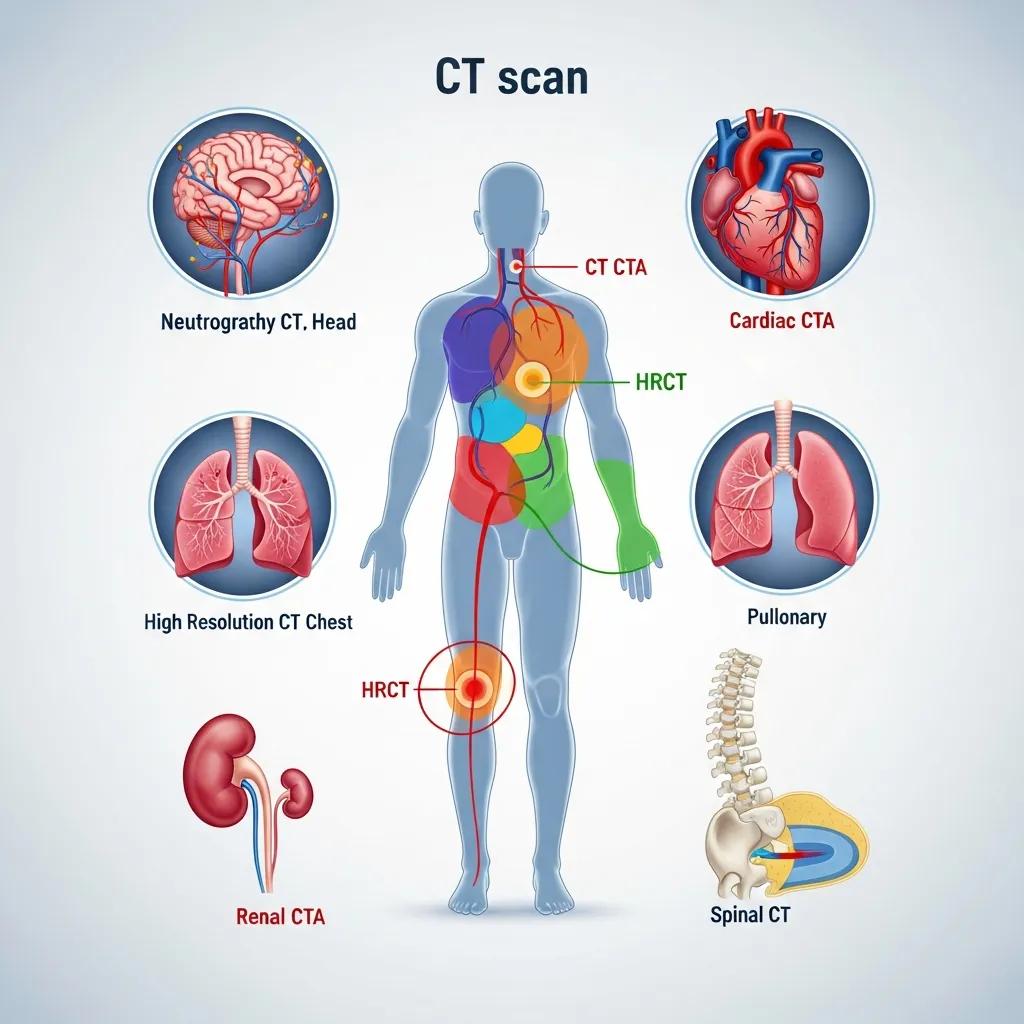
CT protocols are tailored to answer specific clinical questions by adjusting timing, contrast and reconstruction. Common variants include CT angiography (CTA) for vascular mapping, high‑resolution CT (HRCT) for detailed lung assessment, cardiac CT for coronary anatomy and calcium scoring, and CT colonography for large‑bowel evaluation. Contrast‑enhanced CT is used when vascular or soft‑tissue detail matters. In short: CTA for suspected pulmonary embolus or aneurysm; HRCT for interstitial lung disease; cardiac CT for coronary assessment and calcium scoring; CT colonography as a less invasive bowel screen. Special techniques such as cardiac gating synchronise acquisition with the heartbeat to reduce motion, while enteric protocols may include oral contrast to outline bowel loops. These options help referrers choose the most efficient CT variant for each patient.
How Does a CT Scanner Create Detailed Images?
Image formation follows clear steps: projection acquisition, detector capture, analogue‑to‑digital conversion and computational reconstruction into slices. Modern scanners use iterative reconstruction or AI‑assisted methods to improve image quality and reduce noise. Slice thickness and reconstruction kernels set spatial resolution and soft‑tissue contrast — thinner slices reveal small structures but increase data volume. Iodinated contrast increases differences in tissue attenuation, so it’s used to highlight vessels, tumours and inflammation; pre‑scan checks for allergies and kidney function guide safe use. These technical choices affect both diagnostic yield and patient safety, so referrers should specify the clinical question clearly when ordering scans.
When and Why Is a CT Scan Recommended?
CT is recommended when rapid, high‑resolution imaging will change diagnosis or management — for example in trauma, suspected acute intracranial bleeding, evaluation for pulmonary embolus, cancer staging and severe abdominal pain. It’s the preferred modality when bone detail, lung parenchyma or acute haemorrhage must be seen quickly, or when cross‑sectional anatomy will determine urgent intervention. Referrers should weigh the clinical urgency against alternatives when soft‑tissue characterisation without ionising radiation is needed.
The next section lists common indications by organ system to help with referral decisions.
Common clinical scenarios where CT is frequently the investigation of choice include:
- Acute trauma and suspected fractures: rapid detection of complex fractures and internal injury.
- Neurology emergencies: reliable identification of acute intracranial haemorrhage and large infarcts.
- Chest vascular disease: CT pulmonary angiography is the standard test for suspected pulmonary embolus.
- Abdominal emergencies: clear visualisation of perforation, obstruction, abscess and solid‑organ injury.
- Oncology staging: assessment of tumour extent, nodal involvement and distant metastases.
These indications reflect CT’s strengths in speed and spatial resolution. When MRI or ultrasound better answers the clinical question or avoids radiation, those modalities may be preferable. Clear referral wording — stating the clinical question — increases the likelihood of an optimal CT protocol.
Which Conditions Can a CT Scan Detect?
CT identifies a wide range of clinically important conditions by showing differences in tissue density and fine structural detail. It is highly sensitive for fractures, haemorrhage, lung consolidation, solid‑organ injury and many tumours.
In the central nervous system, CT rapidly confirms intracranial bleeding and significant mass effect. In the chest, it detects pulmonary emboli, consolidation and pulmonary nodules. In the abdomen, CT demonstrates perforation, obstruction and inflammatory disease. Limitations include less soft‑tissue characterisation than MRI for some neurological and musculoskeletal problems, and reduced sensitivity for tiny liver lesions without optimised contrast phases. Knowing each system’s strengths helps referrers choose CT when the likely diagnostic yield will influence acute management.
How Does a CT Scan Compare to Other Imaging Tests?
Understanding how CT stacks up against MRI, ultrasound and plain X‑ray clarifies when CT is the most appropriate choice and when alternatives suit better.
Imaging modality comparison for common clinical scenarios.
This comparison shows that CT is often first‑line when rapid cross‑sectional detail is needed; MRI and ultrasound are complementary when radiation avoidance or superior soft‑tissue characterisation is required. Clear clinical questions and context make modality selection more effective.
What Should You Expect During a CT Scan Procedure?
Your CT appointment usually includes check‑in, safety screening for pregnancy and allergies, IV cannulation if contrast is required, positioning on the scanner couch and the scan itself, which takes seconds to minutes. Most appointments are completed within an hour.
Staff will confirm your identity and the reason for the study, review medications and kidney‑related risks if iodinated contrast is planned, and give instructions for breath holds or positioning that help image quality.
Most people experience minimal discomfort beyond lying still; you may hear mechanical noise and feel brief table movement, and technologists will communicate with you throughout.
If contrast is used, short monitoring may follow and you’ll receive advice on hydration and when to seek help if needed.
Practical steps to prepare — simple actions that reduce delays and improve imaging quality — are listed below.
- Bring documentation: Bring your referral, photo ID and any previous imaging if available.
- Medication guidance: Continue most medications unless told otherwise; discuss metformin with your referrer if contrast is planned.
- Fasting instructions: If contrast is required, follow fasting guidance — typically a few hours without food.
- Remove metal and jewellery: Wear comfortable clothing and remove metal objects that can cause artefact.
Following these steps helps ensure the correct protocol is used and reduces cancellations. For booking or detailed pre‑scan advice, contact your imaging provider — they can explain local referral requirements and appointment options.
How Do You Prepare for a CT Scan?
Preparation varies by study and whether contrast is used, but the essentials are consistent: confirm referral details, follow fasting instructions when requested, review medications like metformin, and tell staff about allergies or pregnancy. For contrast studies, we may check renal function beforehand and ask you to stay hydrated unless fasting. Diabetic patients may receive specific instructions for insulin or oral hypoglycaemics. Loose clothing and removing jewellery reduce artefact, and bringing prior imaging helps comparison and can avoid repeat scans. Clear preparation reduces cancellations and ensures diagnostic‑quality images.
What Happens During and After the Scan?
During the scan you lie on a motorised couch that moves through the gantry while the X‑ray tube rotates; technologists communicate by intercom and may ask you to hold your breath to reduce motion.
If IV contrast is given, an injector delivers the agent at a controlled rate; you may notice a warm sensation or metallic taste for a short time. Severe reactions are rare and staff are trained to manage them.
The actual scan phases are rapid — often only seconds — while the total appointment includes preparation and short recovery time.
After the study you can usually resume normal activities and are advised to drink fluids. If you have concerns about delayed symptoms, contact the imaging provider or your referrer.
Is a CT Scan Safe? What Are the Risks and Side Effects?

In short: CT is generally safe when justified clinically, but it does involve ionising radiation and carries a small risk of contrast reactions. When a scan is likely to change management, the benefits usually outweigh the risks.
Radiation exposure varies by examination. Modern scanners and dose‑reduction techniques have significantly lowered effective doses compared with older equipment.
Contrast risks are usually mild — nausea or a warm flush — while true allergic or renal complications are uncommon. Pre‑scan screening and monitoring reduce these risks.
The table below gives typical dose ranges for common CT studies so patients can better understand relative exposure.
This table shows that while CT uses ionising radiation, modern protocols and justification principles aim to keep dose “as low as reasonably achievable” while preserving diagnostic quality. Discuss risks and benefits with your referrer or imaging team so the study chosen is appropriate for your clinical situation.
How Much Radiation Does a CT Scan Involve?
Radiation dose depends on the body region scanned, scanner technology and protocol settings. Head CTs typically have lower effective doses because of skull attenuation, whereas abdominal or multiphase studies usually involve higher doses. For perspective, natural background radiation is about 2–3 mSv per year in many areas, so a single chest CT may approximate a year or two of background exposure.
Common dose‑reduction strategies include automated exposure control, iterative reconstruction, limiting the scanned range and avoiding unnecessary multiphase imaging. If you’ve had multiple prior studies, discuss cumulative exposure with your referrer and consider alternatives where appropriate.
What Are Possible Side Effects or Complications?
Most CT‑related effects are mild and short‑lived: contrast injection can cause warmth, nausea or minor bruising at the cannula site. True allergic reactions range from mild hives to very rare anaphylaxis and are managed promptly at imaging centres.
Kidney injury is a consideration with iodinated contrast, especially in people with pre‑existing renal disease; screening helps reduce this risk.
Serious complications are uncommon. Imaging teams are trained to recognise and treat reactions; if you have a known contrast allergy or significant kidney disease, discuss alternatives or premedication with your referrer. If concerning symptoms occur after a scan — shortness of breath, rash, swelling — seek immediate medical help.
How Are CT Scan Results Interpreted and Used?
Radiologists review CT images in the context of clinical history, technique and prior studies to produce structured reports that guide care. Reports typically include technique, findings with measurements and a concise impression with recommended next steps.
Radiologists prioritise urgent, actionable findings first (for example, haemorrhage or pneumothorax), then provide detailed descriptive findings for the referrer to use in management or staging. Urgent results are communicated immediately to the referrer, while routine reports follow standard turnaround times. The sections below explain who reads images and typical reporting timelines so patients and referrers know what to expect.
Radiologists use a structured reporting approach to ensure clarity and clinical usefulness.
Clear, structured reports reduce ambiguity and speed clinical pathways. Complex cases may also be reviewed in multidisciplinary meetings to refine management plans.
Who Reviews CT Scan Images and What Do They Look For?
Specialist radiologists assess CT images, check technical adequacy, compare with prior imaging when available and identify abnormalities related to the referral question. They prioritise life‑threatening findings for urgent communication. Depending on the indication, radiologists look for haemorrhage, fractures, masses, inflammation, vascular occlusion or contrast leak, and may recommend follow‑up imaging, biopsy or specialist referral. Standardised report sections — technique, findings and impression — keep communication clear for referrers and patients; complex cases are often discussed at multidisciplinary meetings for consensus.
How Long Does It Take to Get CT Scan Results?
Reporting times depend on urgency and provider workflow. Urgent studies such as trauma or suspected stroke are usually reported immediately or within hours, while routine outpatient CT reports commonly take 24–72 hours.
Timing is affected by case complexity, need for subspecialty review and workload. Referrers can request expedited reporting for time‑sensitive cases.
Patients generally receive results through their referring clinician, who will discuss findings and management. If you need faster access, contact your referrer for an expected timeline.
For booking enquiries and referral guidance, remember the service goal: provide clear information about medical imaging services and help with appointments and questions.
For GPs and referrers seeking referral guidance, local protocols and prioritisation criteria are available through established imaging pathways and should be consulted when submitting requests to ensure timely, appropriate imaging.
- Key takeaway: CT provides rapid, high‑resolution cross‑sectional imaging that often changes clinical management in acute and elective settings.
- Action for patients: Tell us about allergies, medications and pregnancy; follow preparation instructions for contrast studies.
- Action for referrers: State the clinical question and preferred protocol to optimise diagnostic yield.
These points summarise practical next steps to help patients and clinicians use CT judiciously and achieve the best outcomes.
Frequently Asked Questions
What should I do if I have a history of allergies before a CT scan?
If you have a history of allergies — especially to iodinated contrast — tell the imaging team and your referrer before the scan. They may recommend premedication or an alternative test that avoids contrast. Sharing details of any previous reactions helps us take appropriate precautions to keep you safe.
Can I eat or drink before a CT scan?
Whether you can eat or drink depends on the type of scan and whether contrast will be used. Many contrast studies require a short fasting period, usually a few hours. Always follow the specific instructions given by the imaging provider, since guidance is tailored to the study and your circumstances.
How long does a CT scan take?
The scanning itself usually takes only a few minutes. Including preparation and any recovery time, expect the full appointment to take up to an hour. The speed of CT is one of its advantages, especially for urgent assessments.
Are there any long-term effects of radiation from CT scans?
CT scans use ionising radiation, and the long‑term risks are generally low when scans are clinically justified. The risk of radiation‑related cancer increases with cumulative exposure, but modern CT protocols aim to minimise dose. Discuss your imaging history with your referrer if you’ve had multiple scans to ensure benefits outweigh risks.
What should I do if I experience discomfort during the scan?
If you feel anxious, uncomfortable or notice symptoms that could indicate a reaction to contrast, tell the technologist right away. They can adjust your position, pause the scan if needed and provide reassurance. If you feel unwell after leaving the centre — severe nausea or breathing difficulty — seek medical attention immediately.
Can I bring someone with me to the CT scan appointment?
Yes — you can usually bring a friend or family member for support. They may not be allowed in the scanning room for safety reasons, especially during active imaging. Check the facility’s visitor policy before your appointment, as some centres limit accompanying persons for space or infection‑control reasons.
What happens if I need a follow-up scan after the initial CT scan?
If a follow‑up scan is needed, your referrer will explain why and when it should occur. Follow‑up imaging is used to monitor change or assess treatment response. Adhering to the recommended schedule helps ensure timely and effective care.
Conclusion
CT scans deliver fast, high‑resolution images that are essential for diagnosis and management in many clinical situations. Understanding how CT works, how to prepare and what the risks are helps you make informed choices about your care. If you’re considering a CT scan, talk with your healthcare provider about your individual needs so we can achieve the best possible imaging outcome. For more information on preparing for an appointment or our services, explore the resources available through your imaging provider.

