CT Scans: A Practical Guide to Uses, Preparation, Types, Benefits and Risks
Computed tomography (CT) uses rotating X‑ray beams and advanced computer reconstruction to produce clear cross‑sectional images of the body. These images help clinicians see internal anatomy quickly and accurately. This guide explains what a CT scan is, how the technology works, and why CT is useful for assessing trauma, cancer, heart and vascular disease, and some neurological emergencies. You’ll find a step‑by‑step outline of what to expect during a scan, practical preparation advice for contrast studies, and a plain explanation of how radiation exposure is measured and reduced with modern low‑dose techniques. We also compare General CT, Cardiac CT and CT Angiography, and include checklists for patients and referrers plus details on booking and eReferral pathways. By the end you’ll understand indications, preparation, benefits, risks and how to arrange a CT with a provider that uses ultra‑low dose, high‑definition CT protocols.
What is a CT scan and how does it work?
A CT scan — short for computed tomography — acquires multiple X‑ray measurements around the patient and reconstructs them into cross‑sectional images using dedicated algorithms. The scanner combines an X‑ray source and detector array mounted on a rotating gantry; data from many angles are processed into contiguous slices that can be viewed in axial, coronal and sagittal planes. CT is valued for its speed and high spatial resolution, making it the investigation of choice in many urgent situations such as major trauma, suspected stroke and severe abdominal pain. The following sections explain the key scanner components and how slices are formed so you can appreciate both the technology and the resulting clinical images.
What technology is used in CT scans?
Modern CT scanners include several core components: an X‑ray tube that emits controlled ionising radiation, a detector array that measures transmitted X‑rays, a rotating gantry that moves those elements around the patient, and reconstruction software that turns raw data into diagnostic images. Contemporary systems also use dose‑management tools and iterative or deep‑learning reconstruction algorithms to reduce noise and maintain image quality at lower radiation doses. ECG‑gating is routinely used for cardiac studies and rapid helical acquisition suits thoraco‑abdominal imaging; protocols are adjusted to answer specific clinical questions. These advances enable ultra‑low dose, high‑definition CT protocols that balance image clarity with patient safety, which is especially important for repeat studies or for more vulnerable patients.
Recent research has examined how deep‑learning reconstruction improves image quality across different dose levels.
Deep Learning Reconstruction for Low‑Dose CT Image Quality
Deep learning reconstruction (DLR) has been introduced by major vendors and evaluated across a range of CT examinations. This study compared DLR with hybrid iterative reconstruction (IR) for standard, reduced and ultra‑low dose CTs (SDCT, RDCT and ULDCT) obtained with high‑definition CT (HDCT), reconstructed at 0.25 mm, 0.5 mm and 1 mm section thicknesses with 512×512 or 1024×1024 matrices in patients with various pulmonary diseases.
Effectiveness of deep learning reconstruction on standard to ultra‑low‑dose high‑definition chest CT images, 2023
How do CT scans produce detailed internal images?
CT collects data as a series of thin slices that are reconstructed and stacked to create a volumetric dataset. This allows multiplanar reformats and 3D renderings that improve anatomical orientation. Contrast media — given orally or intravenously — changes how blood vessels and soft tissues attenuate X‑rays, highlighting lesions, vascular anatomy or active bleeding. Clinicians use windowing and post‑processing tools to emphasise bone, lung or soft‑tissue detail, and modern reconstruction methods help detect small lung nodules and subtle fractures. Combined, these steps produce high‑definition diagnostic images that inform decision making in emergency, oncology and cardiovascular care.
What are the different types of CT scans offered?
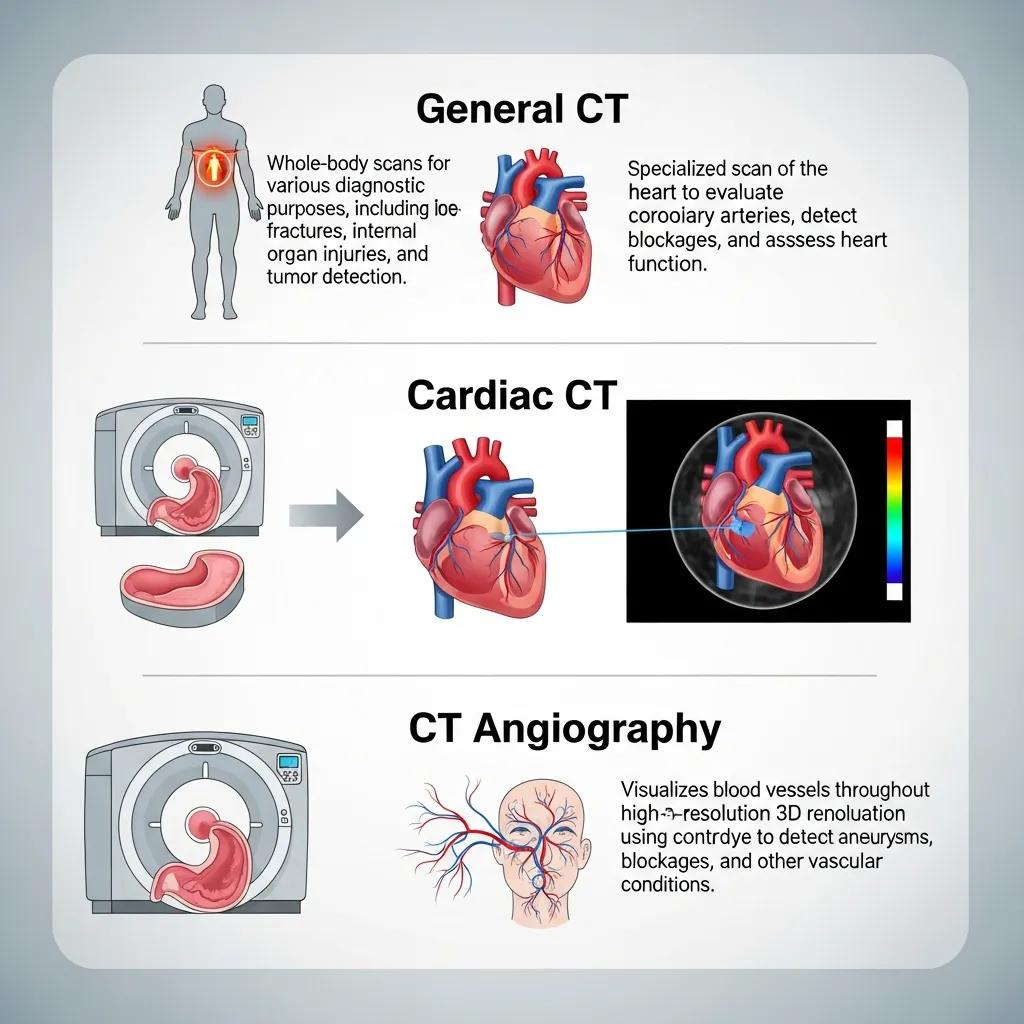
CT covers several specialised study types optimised for different clinical needs: General CT for broad anatomical surveys, Cardiac CT for coronary and structural heart assessment, and CT Angiography for detailed vascular imaging. Which modality is chosen depends on the clinical question — trauma, cancer staging, chest infection, suspected coronary disease or vascular occlusion — because each protocol varies acquisition speed, contrast timing and reconstruction settings.
Different CT types correspond to specific anatomical coverage and indications:
This comparison helps clinicians select the right CT pathway and gives patients a clear expectation of why a particular study is requested.
What is General CT and what body areas does it cover?
General CT is a versatile study used for the head, chest, abdomen, pelvis and extremities. It’s commonly requested for trauma surveys, cancer staging, acute abdominal pain and infection work‑up. Typical indications include detecting intracranial haemorrhage, staging tumours, characterising lung nodules, assessing abdominal inflammation and clarifying complex fractures. A standard General CT appointment involves positioning on the scanner table, possible oral or IV contrast depending on clinical need, and scan times from a few seconds for focused studies to several minutes for contrast‑enhanced abdominal protocols. Its broad scope is why CT is often the first‑line imaging choice when clinicians need a rapid, whole‑region view.
How do Cardiac CT and CT Angiography specialise in heart and blood vessel imaging?
Cardiac CT and CT Angiography use specialised timing, ECG‑gating and contrast protocols to minimise cardiac motion and fully opacify vessels so coronary anatomy, lumen and wall disease are visible. Cardiac CT includes calcium scoring and coronary CTA and may require heart‑rate control (beta‑blockers when appropriate) and breath‑hold instructions to reduce motion artefact. CTA relies on precise contrast bolus timing to highlight arteries or veins of interest. Indications include assessing coronary artery disease risk, investigating chest pain with low‑to‑intermediate pre‑test probability, and pre‑operative vascular planning. Clear instructions about heart‑rate preparation and contrast timing help patients and referrers get ready for these specialised scans.
How should patients prepare for a CT scan?

Good preparation improves image quality and safety whether the study is non‑contrast, uses oral contrast, or requires IV contrast. Preparation depends on the body area and contrast protocol. Patients are usually advised about fasting when IV contrast or abdominal imaging is planned, removing metal objects, and bringing prior imaging and referral documentation. It’s essential to disclose allergies, current medications — particularly metformin — and any chance of pregnancy so the team can assess contrast and renal risks. The checklist and table below offer clear, practical steps for patients and referrers to coordinate pre‑scan requirements.
Patient preparation checklist before a CT scan:
- Confirm the appointment and bring referral documents: Make sure the referral states the clinical question and bring any prior imaging or reports.
- Follow fasting instructions if advised: For many contrast‑enhanced abdominal or pelvic CTs, fasting for a specified period helps image quality.
- Disclose allergies, medications and pregnancy: Tell the radiology team about any previous contrast reactions, medications such as metformin, and if there is any possibility of pregnancy.
Following these steps reduces complication risk and improves diagnostic yield. The table below maps common preparation actions to who they apply to and the usual timing.
Adhering to these preparation steps helps radiographers obtain diagnostic‑quality images and reduces contrast‑related risks.
Current guidance indicates routine pre‑procedural fasting before intravenous iodinated contrast is often unnecessary.
Fasting Guidelines for Contrast‑Enhanced CT Scans
The traditional policy of fasting before contrast‑enhanced CT (CECT) using iodinated contrast media (ICM) lacks strong evidence. Given the potential downsides of fasting, recent guidelines from the European Society of Urogenital Radiology (V10.0) and the American College of Radiology (2021) no longer recommend routine pre‑procedural fasting before standard IV ICM administration.
Preprocedural fasting for contrast‑enhanced CT: when experience meets evidence, 2021
What are the fasting and contrast medium requirements?
Fasting and contrast requirements vary by study. Non‑contrast CTs usually require no fasting, while contrast‑enhanced abdominal or pelvic scans often specify several hours of fasting to reduce aspiration risk and optimise bowel contrast. Oral contrast is given for some abdominal protocols so it reaches the target area at the time of imaging; IV contrast is injected with timed acquisition to highlight vasculature and lesions. Renal function is assessed when IV contrast is planned — recent blood tests may be requested for patients with known kidney disease — and hydration is commonly recommended to help clear contrast. Contacting the radiology team before arrival ensures correct fasting, oral contrast timing and any pre‑scan blood tests are organised.
What important information should patients share before their scan?
Tell the imaging team about any allergies (especially previous contrast reactions), current medications including diabetes treatments like metformin, implanted devices, and any possibility of pregnancy. A concise medical history and recent pathology results let radiologists tailor contrast decisions and, when needed, plan premedication for prior mild reactions. Useful phrases to say at booking or on arrival include: “I’ve had a contrast reaction before,” or “I take metformin for diabetes.” Clear information protects patient safety and helps referrers include essential details on eReferrals so the imaging team can prepare.
What are the benefits and common uses of CT scans?
CT offers fast image acquisition, excellent spatial resolution and broad anatomical coverage, making it central to acute diagnostics, cancer staging and image‑guided procedures. Its speed is vital in emergencies — quickly identifying intracranial haemorrhage in suspected stroke or active intra‑abdominal bleeding after trauma — and its resolution helps detect lung nodules and complex fractures. Ultra‑low dose, high‑definition CT techniques combine iterative reconstruction and dose modulation to lower radiation exposure while preserving diagnostic confidence, which is helpful for follow‑up imaging and screening. The list below summarises the core clinical benefits that make CT a first‑line modality in many pathways.
Key clinical benefits of CT scans:
- Rapid diagnosis: Fast acquisition supports urgent decision making in emergency care.
- High anatomical resolution: Fine detail improves detection of fractures, tumours and vascular disease.
- Versatility across body regions: Tailored protocols let CT assess head, chest, abdomen, pelvis and extremities.
These strengths make CT essential for cancer staging, stroke assessment and trauma management. Below we outline specific clinical examples and how low‑dose options support repeated imaging.
How do CT scans help diagnose cancer, stroke and bone injuries?
CT has distinct roles across oncology, neurology and orthopaedics. In cancer care it provides staging information about tumour size, nodal involvement and metastatic spread. In suspected stroke it quickly excludes intracranial haemorrhage and helps with treatment triage. In trauma, CT detects fractures, organ lacerations and active bleeding. For example, chest and abdominal CT staging guides oncological management by identifying resectable disease or metastatic burden; acute stroke CT protocols are first‑line to differentiate ischaemia from haemorrhage prior to reperfusion decisions; and orthopaedic CT clarifies complex fracture anatomy when plain X‑rays are inconclusive. Choosing the right modality and protocol turns imaging into actionable clinical information.
Ultra‑low‑dose cone‑beam CT is being studied as a lower‑radiation option for certain fracture assessments.
Ultra‑Low‑Dose Cone‑Beam CT for Fracture Assessment
Multi‑detector CT (MDCT) outperforms conventional radiography for fracture detection but involves higher radiation. Cone‑beam CT (CBCT) can offer higher spatial resolution at a lower dose than MDCT, and manufacturers now provide ultra‑low‑dose CBCT algorithms. This study compares diagnostic accuracy of ultra‑low‑dose CBCT (ULDCBCT) with standard‑dose CBCT (SDCBCT) for acute fractures.
Ultra‑low‑dose cone‑beam CT compared to standard dose in the assessment for acute fractures, MC Murphy, 2022
What advantages do ultra‑low dose, high‑definition CT scans provide?
Ultra‑low dose CT techniques reduce radiation using iterative reconstruction, automated exposure control and organ‑based dose modulation while preserving the spatial resolution and contrast needed for diagnosis. Practically, these protocols lower cumulative radiation — important for patients needing serial imaging — without compromising the detection of clinically significant findings such as small lung nodules or subtle bone injury. Clinically, lower doses make surveillance and screening more feasible and reduce theoretical long‑term risks, particularly in younger or more radiosensitive groups. Dose reporting and tracking help clinicians weigh diagnostic benefit against exposure and choose low‑dose protocols when appropriate.
What are the risks and radiation safety considerations of CT scans?
CT involves ionising radiation, so understanding typical dose levels, comparisons with natural background exposure and mitigation strategies is important for informed decisions. Radiation dose varies by study and protocol — for example a head CT differs from a contrast‑enhanced abdominal CT — and modern low‑dose protocols substantially lower exposures. Iodinated contrast carries small risks such as allergic‑type reactions and renal effects in susceptible patients, but screening and preventive measures minimise these events. The table below offers a practical comparison of relative dose ranges and common mitigation methods used to reduce exposure while maintaining diagnostic quality.
This table puts exposure into context and highlights that ultra‑low dose technology and tailored protocols help keep doses at clinically acceptable levels while preserving diagnostic performance.
How much radiation exposure occurs during a CT scan?
Radiation from CT is reported as an effective dose in millisieverts (mSv) and varies by body region and protocol. Many modern low‑dose chest CTs deliver doses comparable to a few months of natural background radiation, while contrast‑enhanced abdominal CTs are typically higher but remain justified when the clinical benefit is clear. Typical ranges for diagnostic CT fall roughly between 1–10 mSv depending on the protocol; iterative reconstruction and dose modulation can substantially reduce these values compared with older scanners. The risk of radiation‑related harm from a single diagnostic CT is generally low, especially when the result directly affects patient care. For repeated imaging, clinicians can choose low‑dose protocols or alternative modalities to balance diagnostic need and safety.
What are the potential risks of contrast medium and pregnancy considerations?
Iodinated contrast media can cause mild to severe allergic‑type reactions in a small number of patients and may affect kidney function in those with pre‑existing renal impairment. Screening questionnaires and eGFR testing where appropriate guide safe administration. Mild reactions include nausea and hives; severe reactions are uncommon but treated immediately by trained staff, and premedication protocols exist for selected patients with prior reactions. Regarding pregnancy, CT is generally avoided unless the maternal benefit outweighs fetal risk; when necessary, pelvic exposure is minimised and alternatives such as ultrasound or MRI are considered. Open communication with referrers about renal function, allergy history and pregnancy status helps ensure the safest imaging pathway.
How can you book a CT scan at Life Medical Imaging Central Coast?
Life Medical Imaging Central Coast provides CT services across multiple Central Coast sites and operates to NATA‑accredited standards using ultra‑low dose, high‑definition CT technology to deliver safe, high‑quality imaging. Patients and referring clinicians can book appointments online or by phone, and referring doctors are supported by an eReferral system that streamlines data transfer and scheduling. After you book, you will receive tailored preparation instructions depending on the CT type and contrast needs; referrers can expect timely reporting and secure delivery of results via established workflows. Our combination of advanced equipment, sub‑specialist expertise in cardiac and women’s imaging, and practical booking pathways helps make access to CT efficient and straightforward.
What online and phone booking options are available?
You can book CT studies using our online appointment system or by phone. Have the referral details, patient identifiers and preferred dates ready so the scheduling team can find a suitable slot and provide preparation instructions. For urgent referrals, calling may allow faster triage and same‑day or next‑available appointments depending on clinical need; online booking is convenient for routine scheduling and after‑hours access to instructions. When booking, confirm whether contrast is required and disclose allergies, medications and pregnancy status so the team can arrange any pre‑scan requirements. Clear guidance at booking reduces delays on the day of the scan and ensures the correct protocol is used.
How does the eReferral system support referring doctors?
Our eReferral system securely transmits referral details, clinical information and prior imaging, speeding up appointment scheduling and reducing transcription errors compared with paper referrals. Referrers should include the clinical question, relevant history and any prior imaging or laboratory results to help the imaging team select the optimal CT protocol and decide if pre‑scan tests are needed. Reports and images are returned electronically through established channels to support timely patient management and continuity of care. This streamlined referral‑to‑report workflow benefits both clinicians and patients by improving coordination and reducing administrative friction.
- Booking options summary:
Online booking: Ideal for routine scheduling and easy access to preparation instructions.Phone booking: Best for urgent referrals and clarifying preparation needs.eReferral: Recommended for referring practitioners to send complete clinical information securely.
These channels work together to provide efficient access to CT imaging and ensure both patients and referrers receive clear guidance before and after the scan.
Frequently Asked Questions
What should I expect during a CT scan procedure?
During a CT scan you lie on a motorised table that moves through a large, ring‑shaped scanner. The scan itself is quick — often just a few minutes — and you may be asked to hold your breath briefly to reduce motion blur. Some studies require contrast given orally or via an IV to improve image clarity. The radiology team will explain each step and ensure your comfort and safety throughout the procedure.
Are there alternatives to CT scans for imaging?
Yes. Alternatives include MRI (magnetic resonance imaging) and ultrasound. MRI uses magnetic fields and radio waves and is especially useful for soft‑tissue detail, while ultrasound uses sound waves for real‑time imaging of organs and blood flow. Each modality has advantages and limitations; your clinician will recommend the most appropriate test based on the clinical question and your circumstances.
How often can I safely undergo a CT scan?
How frequently you can have a CT depends on clinical need and individual circumstances. CT involves ionising radiation, so for patients needing multiple scans clinicians weigh risks and benefits and often use low‑dose protocols where suitable. Always discuss your imaging history and any concerns with your referrer so the team can choose the safest appropriate option.
What are the signs of a contrast medium reaction?
Contrast reactions range from mild to, rarely, severe. Mild symptoms include nausea or a skin rash. Severe reactions — uncommon — can include difficulty breathing, facial or throat swelling, or a rapid heartbeat. If you notice any unusual symptoms after contrast administration, tell staff immediately; they are trained to manage reactions. Always disclose known allergies or prior contrast reactions before your scan.
Can I eat or drink before a CT scan?
Whether you can eat or drink depends on the type of study. Non‑contrast scans generally have no restrictions. If your scan involves IV contrast or focuses on the abdomen/pelvis, you may be asked to fast for a few hours beforehand. Follow the specific instructions we provide to ensure the best possible images.
What happens after the CT scan is completed?
After your CT you can usually return to normal activities immediately unless advised otherwise. If you received contrast, you may be asked to drink extra fluids to help clear it. A radiologist reviews the images and prepares a report for your referring doctor. Timing for results varies with urgency, but routine reports are typically available within a few days. Your clinician will discuss the findings and any recommended follow‑up.
Conclusion
CT scanning delivers fast, high‑resolution imaging that plays a vital role in diagnosing conditions from trauma to cancer. Modern, ultra‑low dose protocols help keep radiation exposure low while preserving diagnostic accuracy. Knowing how to prepare and how to book a study makes the process smoother for patients and referrers. To learn more about CT or to book an appointment, explore our services or contact our team today.

