CT Scans Explained: Benefits, Safety, Technology and How to Prepare
Computed tomography (CT) creates detailed cross-sectional pictures of the body by combining rotating X-ray beams with detector arrays and computer reconstruction. It delivers fast, high-resolution images that help clinicians diagnose conditions and plan treatment. This guide covers how CT works, the situations where it’s most useful, how modern low-dose techniques lower radiation exposure, and what patients can expect before, during and after a scan. You’ll also find clear comparisons with MRI, X-ray and ultrasound, practical checklists for general and cardiac CT preparation, and an accessible summary of recent technical advances like AI reconstruction and photon-counting detectors. Finally, we explain how Central Coast patients and referrers can access CT services at Life Medical Imaging Central Coast and how to book an appointment. Read on for clinical examples, dose comparisons, preparation steps, technology context and simple booking guidance for patients and clinicians.
When is CT most useful — key benefits and common uses
CT is a rapid, cross‑sectional imaging tool that uses X‑ray transmission and computer reconstruction to show bone, air, soft tissue and blood vessels in fine detail. By collecting multiple projections and assembling thin slices, CT allows multiplanar views and 3D reconstructions — features especially valuable in emergencies, cancer staging and vascular assessment. For patients, CT’s main advantages are quick scans, excellent bone and lung detail, non‑invasive vascular imaging with CT angiography and the ability to inform urgent clinical decisions. These strengths make CT the go‑to test in many acute situations where timely, reliable information affects care.
Common clinical uses of CT across body systems include:
- Trauma assessment to detect internal bleeding and fractures that require urgent surgery.
- Chest imaging for pneumonia, pulmonary embolism and lung nodule evaluation.
- Abdominal CT to investigate bowel obstruction, appendicitis and intra‑abdominal sepsis.
- Cancer staging and follow‑up to measure tumour size, spread and response to treatment.
These examples lead into a clear table summarising common CT types and their primary advantages for specific problems.
Different CT exams answer different clinical questions; the table below summarises common CT use‑cases and the main benefits of each.
This table explains why clinicians select particular CT protocols and prepares you for the following sections on diagnostic mechanisms and cardiac CT.
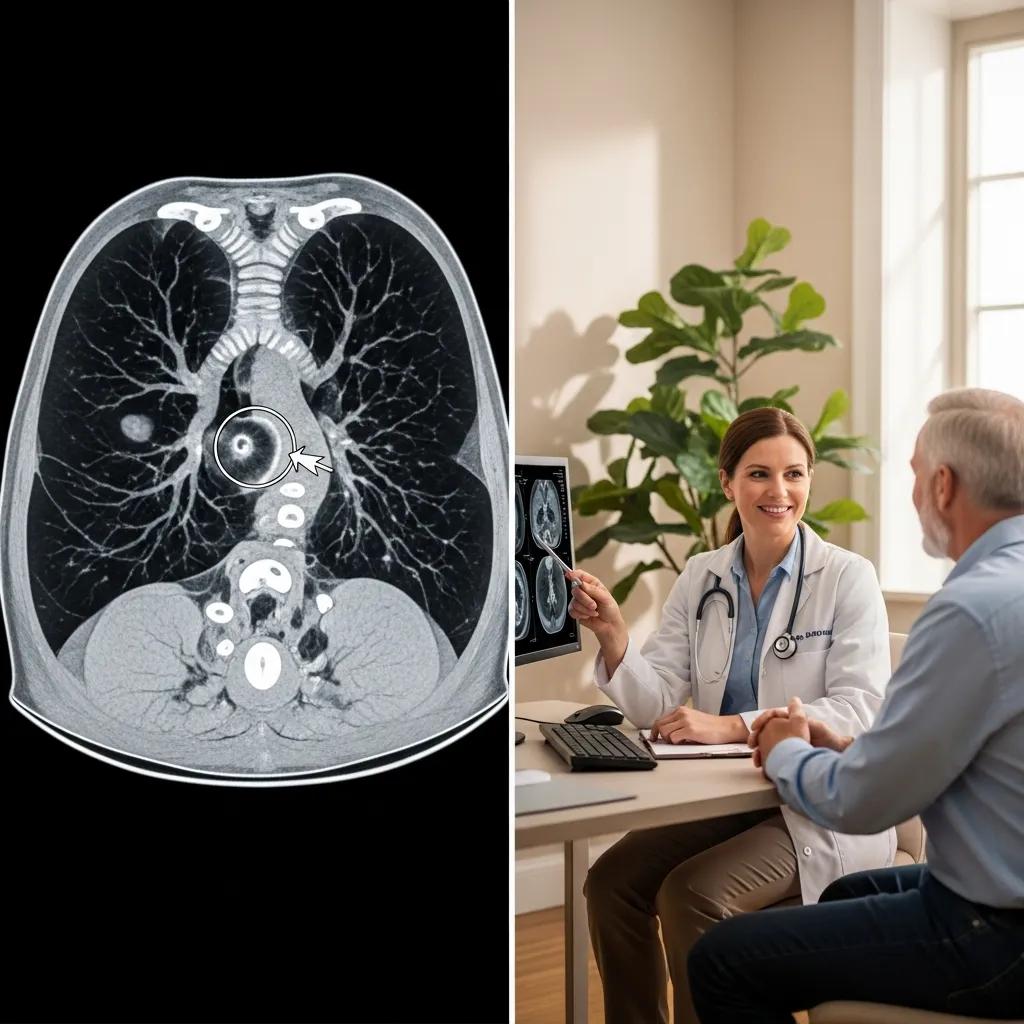
How CT scans help diagnose medical conditions
CT produces cross‑sectional images that highlight tissue density differences and patterns of contrast enhancement, allowing clinicians to spot bleeding, fractures, tumours and blocked vessels. Rapid capture of many thin slices enables multiplanar reconstructions — axial, sagittal and coronal — for precise localisation. For example, in trauma a whole‑body CT can quickly reveal life‑threatening haemorrhage, organ laceration or pelvic fractures that plain X‑rays may miss, speeding up surgical decisions. These diagnostic strengths explain CT’s role as a first‑line test in many acute care settings.
Radiologists combine attenuation measurements, contrast enhancement behaviour and anatomical relationships to distinguish pathologies and guide treatment. The next section describes cardiac CT and CT angiography and the patient benefits they offer.
Why use cardiac CT and CT angiography?
Cardiac CT and CT angiography image the coronary arteries and cardiac structures non‑invasively using ECG gating and timed contrast injection to reduce motion and highlight vessels. These studies support coronary calcium scoring for risk assessment, accurate evaluation of coronary stenosis, and pre‑procedural planning for stenting or surgery. For selected patients, cardiac CT can avoid the risks of invasive angiography and complements functional tests by showing precise anatomy. For people with chest pain and intermediate risk, cardiac CT can rapidly identify who needs invasive assessment and who may be managed conservatively.
CT angiography also maps vessels elsewhere — pulmonary, cerebral and peripheral arteries — helping plan endovascular procedures and guide urgent care. That leads into the next topic: radiation safety and dose reduction.
How safe are CT scans? Radiation exposure and modern low‑dose methods
CT uses ionising radiation to create images. Understanding dose, risk and ways to reduce exposure helps patients and clinicians weigh benefits against possible harms. Ionising radiation deposits energy in tissue and can slightly increase lifetime cancer risk in a stochastic (probabilistic) way, but the absolute risk from most diagnostic CT scans is small compared with the clinical benefit when the result changes management. Current CT practice emphasises justification — only scanning when clinically indicated — and optimisation — keeping dose as low as reasonably achievable while maintaining image quality. Newer technology supports substantial dose reductions without losing diagnostic confidence.
To provide perspective, the table below compares typical effective doses for common imaging studies and everyday background radiation.
Giving clear dose figures helps patients and referrers understand scale and supports shared decision‑making about imaging.
What is ionising radiation and how can it affect patients?
Ionising radiation consists of energetic photons or particles that can remove electrons from atoms and trigger chemical changes, including DNA damage that may increase cancer risk over time. Effects are described as deterministic (dose‑threshold effects like skin burns — rare in diagnostic imaging) and stochastic (a small, probabilistic rise in cancer risk with cumulative dose). For diagnostic CT the main concern is stochastic risk, which increases gradually with dose; however, the small absolute increase must be balanced against the immediate benefit of an accurate diagnosis. Clinicians use risk‑benefit considerations and patient factors — such as age and pregnancy — when deciding whether a CT is appropriate.
This is why dose‑reduction technology and patient‑specific protocols are central to modern CT practice, which we discuss next.
How ultra‑low dose CT technology reduces radiation
Lowering dose combines better hardware, advanced reconstruction algorithms and optimised protocols to keep image quality high at reduced exposures. Iterative reconstruction and AI‑based denoising clean raw data to remove noise while preserving detail, enabling lower tube current or voltage settings. Photon‑counting detectors — an emerging detector technology — offer improved dose efficiency through direct energy discrimination. Protocol optimisation also includes automated exposure control, accurate patient positioning and narrowing the scanned volume to the area of interest. Together, these measures reduce cumulative exposure, especially for patients needing repeated scans.
At Life Medical Imaging Central Coast we follow established best practices: using ultra‑low dose protocols where clinically appropriate, applying iterative reconstruction and tailoring scan parameters to patient size and indication, and using specialised cardiac protocols that balance temporal resolution and dose. Next, we cover how to prepare for your CT to ensure safe, high‑quality images.
Preparing for a CT scan — a practical guide
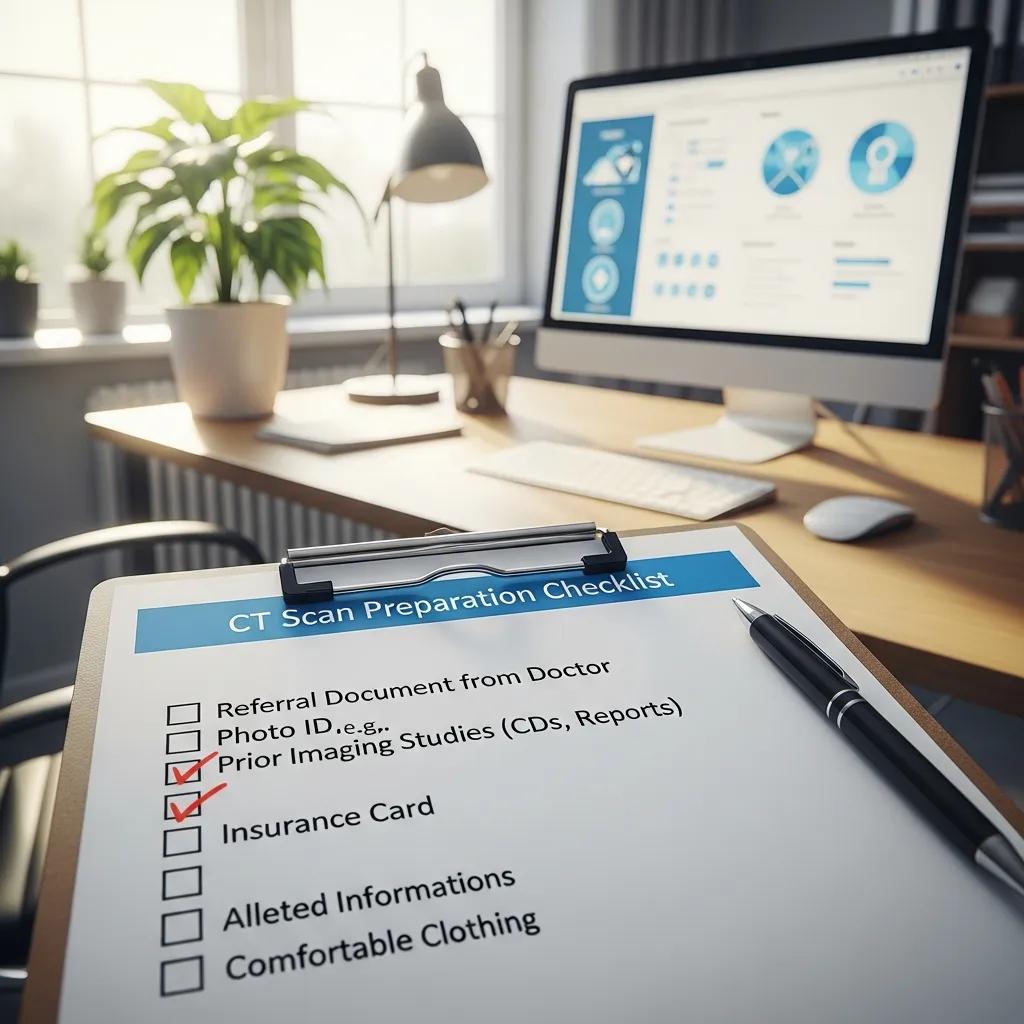
Good preparation improves image quality, reduces the need for repeat scans and lowers risks associated with contrast. Preparation varies by CT type — general, abdominal or cardiac — and may include fasting, medication adjustments and declaration of allergies or kidney problems. Bring your referral, ID and any prior imaging for comparison; follow staff instructions on breath‑holding and removing metal to avoid artefact. Clear preparation reduces stress and helps the appointment flow smoothly from registration to image acquisition.
Below are practical checklists for common CT preparations so patients know what to expect and clinicians can give consistent instructions.
Common preparation steps for general and abdominal CT:
- Fast for 2–6 hours if oral or intravenous contrast is planned — follow the specific instructions we give you.
- Bring your referral, photo ID and any previous imaging or surgical reports for comparison.
- Remove jewellery, metal hair accessories and clothing with metal fasteners to avoid image artefact.
- Tell staff if you are pregnant, have had a reaction to contrast before, or take medications such as metformin or blood thinners.
These basic steps apply to most outpatient CT exams. Cardiac‑specific preparation is outlined next.
Preparation for general and cardiac CT scans — what’s different?
General CT preparation focuses on reducing artefact and ensuring safe use of contrast: fasting where needed, checking kidney function and allergy history, and temporarily withholding certain medicines as instructed. Cardiac CT often requires controlling the heart rate for clearer images; this may involve pre‑scan beta‑blockers when appropriate, avoiding caffeine beforehand and following fasting guidelines to limit motion. Referrers and patients should tell staff about comorbidities — especially asthma, diabetes or kidney disease — so contrast dosing and monitoring can be tailored. Good preparation reduces repeat imaging and supports accurate diagnosis.
Next we describe what happens during the scan so patients know what to expect.
What to expect during your CT appointment
A typical outpatient CT visit includes registration, a brief clinical checklist and consent, positioning on the scanner table and one or more short image acquisitions — often seconds to a few minutes depending on the protocol. A radiographer will explain breath‑hold instructions and what sensations to expect, such as a warm flush when intravenous contrast is injected; staff monitor you throughout and are available for questions. After the scan, observation is usually short for contrast studies, and a radiologist reports the images with results sent to your referring clinician. Knowing the sequence of events lowers anxiety and helps you follow instructions for the best possible images.
Recent advances in CT technology
New CT developments focus on higher resolution, spectral information and dose efficiency while speeding reconstruction and workflow. Key areas include AI‑driven reconstruction and post‑processing, iterative reconstruction, dual‑energy and spectral imaging, and the clinical rollout of photon‑counting detectors that discriminate photon energies at the detector.
These technologies deliver clearer images at lower doses, better tissue characterisation, reduced metal artefact and faster availability of images for reporting. Together they support more confident diagnoses and more targeted patient care.
How AI improves image quality and diagnostic speed
AI helps CT by enabling smarter denoising, faster iterative reconstruction and automated post‑processing that measures anatomy and flags urgent findings for the radiologist. Trained machine‑learning models reduce noise while preserving subtle structures, allowing lower acquisition doses without losing diagnostic detail. AI also speeds workflow by automating measurements (for example, tumour volumes), creating reformats and prioritising studies that need urgent review. These gains shorten time‑to‑report and improve consistency, benefiting both clinicians and patients through faster decisions.
That leads into photon‑counting CT, a hardware advance that complements AI improvements.
What is photon‑counting CT and why it matters
Photon‑counting CT uses detectors that count individual X‑ray photons and measure their energy, giving higher intrinsic spatial resolution and spectral information without the cross‑talk seen in traditional energy‑integrating detectors. This improves contrast‑to‑noise, enhances material separation (for example iodine versus calcium) and increases dose efficiency by extracting more information from each photon. While still becoming common in routine practice, photon‑counting promises better visualisation of small structures and finer lesion characterisation. Clinically, this trend means higher quality images at lower radiation doses — a benefit we expect Central Coast clinics to adopt more widely over time.
Photon‑counting detector CT represents an important technological step forward in imaging capability.
Photon‑Counting Detector CT: Technical advancements and benefits
Since Hounsfield’s first CT system in 1971, most clinical CT scanners have used scintillating energy‑integrating detectors (EIDs) that convert X‑ray energy to visible light and then to an electronic signal. An alternative is a one‑step, direct X‑ray conversion approach using energy‑resolving, photon‑counting detectors (PCDs). PCD‑CT has been studied extensively, with early clinical advantages reported from investigational systems. The first commercial clinical PCD‑CT system became available in 2021. Compared with EIDs, PCDs offer higher spatial resolution, improved contrast‑to‑noise ratios, elimination of electronic noise, better dose efficiency and routine multi‑energy imaging. This review provides a technical introduction to PCD‑CT and outlines benefits, limitations and potential improvements.
Life Medical Imaging Central Coast keeps pace with contemporary CT capabilities — offering ultra‑low dose protocols, high‑definition general CT and specialist cardiac CT/CT angiography at our Central Coast sites. Patients can access these services via local appointments and referral pathways. The next section compares CT with other imaging options to clarify when CT is the preferred choice.
How CT compares with other imaging: MRI, X‑ray and ultrasound
CT, MRI, X‑ray and ultrasound each have roles determined by the clinical question, patient factors and availability. CT is fast and excellent for bone, lung detail and vascular imaging with CT angiography. MRI gives superior soft‑tissue contrast without ionising radiation and is preferred for brain, spinal cord and soft‑tissue problems. X‑ray is quick and low dose for initial bone assessment. Ultrasound is portable, radiation‑free and ideal for real‑time assessment of fluid and obstetric imaging. Knowing these differences helps referrers choose the right test and helps patients understand what each modality can and cannot show.
The table below gives a quick comparison to guide decision‑making.
This quick reference helps choose the right test and precedes targeted comparisons between CT and MRI and scenarios where CT is preferred over X‑ray or ultrasound.
CT versus MRI — the main differences
CT uses X‑rays and is strong for bone, lung imaging and fast assessment in emergencies. MRI uses magnetic fields and radiofrequency pulses to provide superior soft‑tissue contrast without ionising radiation. CT scans are usually much shorter than MRI, so CT is preferred for acute or unstable patients; MRI is chosen for detailed evaluation of the brain, spinal cord, ligaments and soft‑tissue tumours. Contraindications differ: MRI may be unsuitable for patients with certain implants or severe claustrophobia, while CT involves radiation that is a consideration in younger patients and for repeated studies. These differences guide modality choice based on the clinical question and patient‑specific risks.
Next, practical scenarios where CT is the right choice compared with X‑ray or ultrasound.
When CT is preferred over X‑ray or ultrasound
CT is the preferred test when three‑dimensional detail, high spatial resolution or a comprehensive body survey is required — for example complex fractures, polytrauma, suspected visceral injury or vascular pathology that exceed the diagnostic limits of X‑ray or ultrasound. CT angiography gives non‑invasive arterial maps that ultrasound cannot reliably achieve in many vascular territories, and CT is more sensitive than plain films for intra‑abdominal free air or subtle bowel injury. While X‑ray and ultrasound remain invaluable for focused, bedside or pregnancy imaging, CT is the decisive tool when full anatomic detail and fast whole‑body assessment are needed. These distinctions help referrers choose the most appropriate imaging for patient care.
The direct conversion and energy‑resolving features of photon‑counting detectors deliver clear advantages in image quality and dose efficiency.
Clinical applications of photon‑counting detector CT: enhanced image quality and dose efficiency
The X‑ray detector is a core component of a CT system that determines image quality and dose efficiency. Until the approval of the first clinical photon‑counting detector (PCD) system in 2021, clinical CT scanners used scintillating detectors that do not capture individual photon information in a single step. PCDs use a one‑step process where X‑ray energy is converted directly into an electrical signal, preserving information about individual photons and allowing energy‑range counting. Key advantages include elimination of electronic noise, improved dose efficiency, increased iodine signal, the potential to reduce contrast volume, and better spatial resolution.
How to book a CT scan at Life Medical Imaging Central Coast
Booking at Life Medical Imaging Central Coast is straightforward for patients and referrers. CT services are available across multiple Central Coast sites. Referrals from GPs or specialists determine the appropriate CT protocol; please bring your referral, photo ID and any prior imaging to the appointment. To book or ask questions, call 02 4326 7000 or use the clinic website booking options; our staff will advise on preparation, contrast needs and whether pre‑scan tests (for example kidney function blood tests) are required. We follow safety practices including dose optimisation and, when needed, premedication or monitoring for contrast reactions.
Where on the Central Coast can you get CT imaging?
- Bateau Bay: Outpatient imaging with standard CT protocols suitable for general and chest/abdominal studies.
- Killarney Vale: Community site offering high‑definition CT imaging and streamlined appointments.
- Umina Beach: Convenient coastal location providing general CT services and patient‑focused scheduling.
- Erina: Central clinic with specialist cardiac imaging and CT angiography capability.
How to schedule your appointment and what to bring
To schedule, call 02 4326 7000 and our team will explain required referral documents, preparation steps and suggested arrival times. You can also use the clinic website booking portal for convenience. On the day, bring the written referral, photo ID, Medicare card if applicable, a list of current medications and any prior imaging. For contrast studies, bring recent lab results if requested (for example renal function) and inform staff about allergies. Arrive 10–20 minutes early to complete registration and expect a short consent discussion with the radiographer; clear communication about your health history allows the team to tailor the protocol safely.
Quick checklist — what to bring to your CT appointment:
- Referral from your GP or specialist.
- Photo identification and Medicare card (if applicable).
- Any prior imaging or reports for comparison.
- List of current medications and any allergy history.
- Recent blood results if required for contrast safety.
Following these steps helps avoid delays and ensures the imaging team can personalise your scan safely and effectively.
Radiologists can gain new insights from photon‑counting CT because of its higher spatial resolution, improved iodine signal and reduced artefacts.
Photon‑counting detector CT: key points radiologists should know
Photon‑counting detector (PCD) CT is a novel detector technology that directly converts incident X‑ray photon energy into electrical signals. The detector design enables smaller pixel sizes for improved spatial resolution and count weighting that boosts iodine signal, while also supporting multi‑energy imaging. PCD‑CT can eliminate electronic noise and reduce artefacts through energy thresholds. Improved dose efficiency is particularly valuable for low‑dose and paediatric imaging. The ultra‑high spatial resolution of PCD‑CT supports lower‑dose scanning across anatomical regions and is useful for critical findings in thoracic and musculoskeletal CT. Enhanced iodine signal may improve low‑contrast tasks in abdominal imaging.
Frequently asked questions
What should I do if I have a history of allergies to contrast media?
If you have known allergies to contrast agents, tell the imaging team before your scan. We may take extra precautions such as premedication with antihistamines or steroids to reduce reaction risk, or recommend an alternative imaging test if safer. Your clinical history will guide the team’s plan — always report any previous contrast reactions so we can keep you safe.
How long does a typical CT scan take?
Most CT scans take only a few seconds to a few minutes to acquire images. Total appointment time, including registration and preparation, is commonly between a few minutes and about 30 minutes depending on the study and whether contrast is used. Allow extra time for paperwork and observation if contrast is administered.
Are there specific risks for pregnant women?
CT uses ionising radiation, which can pose a risk to a developing fetus. If you are pregnant or think you might be, tell your referring clinician and the imaging staff before booking. Often we can recommend alternatives such as ultrasound or MRI that avoid radiation. If a CT is essential, we take steps to minimise exposure, for example using the lowest practicable dose and shielding where appropriate. Discuss risks and benefits with your doctor.
Can I eat or drink before my CT scan?
Whether you should eat or drink depends on the type of CT. For scans involving oral or intravenous contrast, fasting for about 2–6 hours is commonly advised. Follow the specific instructions provided by the imaging centre. If you’re unsure, contact our booking team for guidance.
What happens if I need a repeat CT scan?
If a repeat CT is needed, your clinician will consider whether it’s justified based on your condition and prior images. Repeat studies may be required to monitor progress or investigate new symptoms. If you’re concerned about radiation, ask your doctor to explain how the benefits outweigh the small additional risk. Modern scanners and protocols often reduce dose for follow‑up studies.
How can I access my CT scan results?
After your CT, a radiologist reviews the images and prepares a report that is sent to your referring clinician. Your doctor will discuss the results with you. Some facilities also provide access via an online patient portal — check with our team if this is available. If you have questions about your report, contact your referring clinician for clarification.
What should I do if I feel uncomfortable during the scan?
If you feel anxious, uncomfortable or in pain during the scan, tell the radiographer right away. Our staff are trained to help — from repositioning you to offering calming techniques. In some cases, sedation can be arranged for patients with severe anxiety. Your comfort and safety are our priorities, so please speak up if you need assistance.
Conclusion
CT provides rapid, high‑resolution imaging that supports timely and effective clinical decisions across many situations. Advances such as low‑dose protocols and AI‑assisted reconstruction improve safety while preserving image quality. Knowing how to prepare and how to book a scan at Life Medical Imaging Central Coast will help your visit run smoothly. For more information about our CT services or to make an appointment, visit our website or call us today.

